Atherosclerosis Without Cardiovascular Risk Factors
This study, a sub-population of the PESA study, clearly shows that Atherosclerosis Without Cardiovascular Risk Factors occurs far sooner than we often think. This paper, published in the Journal of the American College of Cardiology, is entitled “Normal LDL-Cholesterol Levels Are Associated With Subclinical Atherosclerosis in the Absence of Risk Factors.” It was conducted on a subset of participants in the larger PESA Study. The title implies that it doesn’t matter if your LDL is elevated or not, you still may be at risk for developing plaque in your arteries. In other words, we miss a lot of patients at risk for heart attacks when we are looking at the typical risk factors often described in traditional medicine.
We typically consider patients to be at low risk of cardiovascular disease and heart attacks if they don’t have the typical CardioVascular Risk Factors (CVRF) such as:
- Smoking
- Hypertension (BP >140/>90)
- Fasting blood sugar >126 mg/dL
- Total Cholesterol >240 mg/dL
- LDL Cholesterol >160 mg/dL
- HDL <40 mg/dL
In this paper, there was a sub-group of patients considered to have Optimal Risk Factors. This means that the patients were the “best of the best” so to speak, in regards to their risk factors for cardiovascular disease. The “optimal risk factors” were defined as follows:
- Blood pressure <120/<80
- Fasting glucose <100 mg/dL
- Glycosylated Hemoglobin (A1c) <5.7%
- Total cholesterol <200 mg/dL
The traditional approach to assessing risk for cardiovascular disease is based on RISK FACTORS as defined above. The question is “does assessing for these risk factors help prevent cardiovascular disease?” The authors of this study attempted to answer this question.
First, they assessed patients for the “typical cardiovascular risk factors” as defined above. The investigators then performed ultrasound to detect carotid, iliofemoral, and abdominal aortic plaque; coronary artery calcification (CAC) score; serum biomarkers; and lifestyle in order to detect atherosclerosis and cardiovascular disease.
In my experience, most cardiovascular disease evaluation is based on risk factors (as listed above) and symptoms. If you are considered very high risk then you MAY get some additional work-up but it is often difficult to get it approved my insurance. However, if you have symptoms then it is much more likely that insurance will cover the additional workup. The bottom line is that you don’t get worked up until you have disease so bad that you are seriously obstructing the artery. This simply makes ZERO sense!
What is even worse is that 68% of heart attacks occur in patients with less than 50% blockage2 in their arteries. These lesions probably wouldn’t show up on stress tests anyway! We are doing a TERRIBLE job at identifying cardiovascular disease early in its inception when it would be easiest to treat and monitor.
Atherosclerosis without Cardiovascular Risk Factors – Methods
As mentioned earlier, the group in this study is a sub-population from the Progression of Early Subclinical Atherosclerosis (PESA) Study. This population had CardioVascular Risk Factors (CVRF) below the current recommended thresholds. 4,184 participants were screened ranging from 40-54 years of age. Exclusion criteria were: known cardiovascular disease, actively being treated for cancer, or any disease where their life expectancy or ability to maintain study protocol were compromised. 4,027 (96.2%) participants had all of the required data available. 1,779 (42.5%) participants (50.3% were women) were in the CardioVascular Risk Factor (CVRF) Free population. 740 (41.6%) of those participants had CardioVascular Risk Factors at optimal levels.
At baseline, each participant went through a clinical interview, evaluations (lifestyle and activity), physical exam, EKG, and imaging studies. These were repeated at 3 and 6 years.
The study population had no CardioVascular Risk Factors as defined above. The study population represented 42.5% of the PESA study group in total. As mentioned above, there was another sub-group with “optimal” CardioVascular Risk Factors (CVRFs) which were also defined above. Other risk factors were defined as follows:
- Family History of CVD: 1st-degree relative with clinical atherosclerosis (men <55 yrs of age, women <65 yrs of age)
- Obesity: BMI >30 kg/m2
- No tobacco use
The 10-year risk of atherosclerotic cardiovascular disease was calculated as follows:
- Low: <5%
- Intermediate: 5 to <7.5%
- High: > 7.5%
The 30-Year Framingham Risk Scores (FRS) were calculated and classified as follows:
- Low: <10%
- Moderate: 10-20%
- High: >20%
Blood samples were obtained and tested for:
- Total Cholesterol
- HDL
- LDL (calculated by the Friedwald equation)
- oxLDL
- Triglycerides
- Lp(a)
- Glucose
- Insulin
- AbA1c
- Cystatin C
- Creatinine
- hs-CRP
- Fibrinogen
- VCAM-1
- P-selectin
Physical activity was monitored with an ActiTrainer accelerometer for 7 consecutive days. The PREDIMED Score was also calculated in order to assess Traditional Mediterranean Diet (TMD) compliance.
Assessment for Subclinical Atherosclerosis
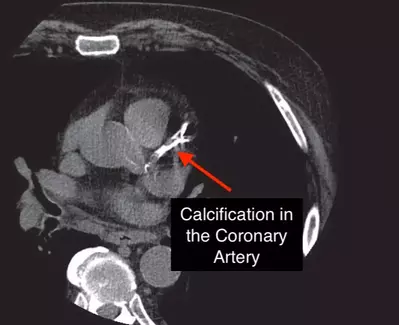
Vascular Ultrasound (2D) and CT (non-contrast) performed as noted previously. Plaque was defined as a localized protrusions into the lumen of the artery with a thickness of either more than 0.5mm or 50% of the intima-media thickness (IMT). Diffuse intima-media thickness of >1.5mm.
The Coronary Artery Calcium Score (CAC) was obtained by the Agatston method. All of the CT scans were analyzed at Imaging Core Laboratory by blinded radiologists.
Subclinical Atherosclerosis was defined as either a CAC of >1 or vascular ultrasound score of >1. Participants were score as:
- Disease Free: 0 vascular sites affected
- Focal Atherosclerosis: 1 vascular site affected
- Intermediate Atherosclerosis: 2-3 vascular sites affected
- Generalized Atherosclerosis: 4-6 vascular sites affected
Results
Even though there were no conventional CardioVascular Risk Factors, 49.7% of the participants had clinical atherosclerosis.
- 46.7% had peripheral vascular disease (PAD)
- 22.7% had plaque in their coronary arteries
- 17.2% had plaque in their abdominal aorta below the renal arteries
- 30.1% had plaque in the iliofemoral arteries.
- 11.1% had coronary artery calcium, most of them were mild (CAC of <100).
The extent of atherosclerosis analysis showed:
- 22.6% had Focal Atherosclerosis
- 20.9% had Intermediate Atherosclerosis
- 6.0% had Generalized Atherosclerosis
For participants in the Optimal CVRF group:
- 280 (37.8%) had atherosclerosis (peripheral plaques in 268, CAC in 43)
- 20.8% had Focal Atherosclerosis
- 13.8% had Intermediate Atherosclerosis
- 3.2% had Generalized Atherosclerosis
So, even though the risk factors were OPTIMAL, there was STILL cardiovascular disease present. We simply can’t trust these risk factors alone for evaluating your risk of having a heart attack!
Presence of Atherosclerosis Prediction (and multi-territorial extent)
There were significant associations between the extent of atherosclerosis as well as its presence with all measured variables except for Family History, Lp(a), Cystatin-C, hs-CRP, and Fibrinogen. VCAM-1 was not associated with the presence of plaque but was associated with its extent. Age, gender, HbA1c, and LDL were associated with the presence of disease in multivariable models. The extent of atherosclerosis was associated with the same variable as well as VCAM-1 and Cystatin-C.
Age, male gender, and LDL were associated with both the presence and extent of disease in the group with Optimal CVRFs.
There was a linear relationship with the presence of atherosclerosis and LDL. The higher the LDL, the more likely there was atherosclerosis. In the group with LDL of 60-70, the incident of atherosclerosis was 11%. However, incidence increased to 64% in the 150-160 group.
Atherosclerosis without Cardiovascular risk factors? Discussion:
The traditional approach to evaluating your risk for cardiovascular disease is based on risk factors. This type of evaluation is simply not effective. Do YOU want to know if you have cardiovascular disease? Are you okay with the fact that your doctor may miss it half of the time?
I’m not okay with this!
It is NOT okay that we miss so many potential heart attacks. I want to know for sure that I am at risk or I’m not. This is why we developed the CardioHealth 101, Advanced, and Platinum screening programs. These assessments for cardiovascular disease evaluate, not only your risk factors but also your actual disease. We use similar testing (and many more of them) to accurately and comprehensively evaluated your risk for actually having a heart attack.
There are many reasons for the multiple findings in this study. LDL was associated with increase risk of atherosclerosis as well as age and gender. Regardless of the CAUSE of atherosclerosis, which is not LDL, its presence is NOT clearly defined by the current recommendations for these risk factors. It is important that we look at the disease process and work to limit the effect of each step.
Additionally, it is important that we are more aggressive with risk and disease screening as early as possible and aggressively intervene when disease is identified we can clearly get atherosclerosis without cardiovascular risk factors.
References
- J Am College of Cardiology 2017;70(24):2979-91
- Circulation. 1995;92:657–671