Arterial Remodeling With Hypertension
We know that hypertension is associated with an increased risk of cardiovascular disease. In fact, it is the #1 contributor to cardiovascular disease.
We also know that hypertension is caused by a number of different mechanisms that result in elevated blood pressure. The blood vessel responds appropriately in an attempt to protect the fragile capillaries and prevent them from blowing out due to this increased pressure.
Unfortunately, many medications traditionally employed for the treatment of hypertension do not address the sick artery. A medication is prescribed and blood pressure improves some so it appears to be successful. However, there is no measurement of, or even thought about, improving arterial health and function. Hydrochlorothiazide (HCTZ) is an excellent example of a drug that doesn’t help anything at all.
In order to improve health and reduce cardiovascular disease risk we need to consider the process occurring in the artery and the therapies that will reverse this process and return the artery to normal function.
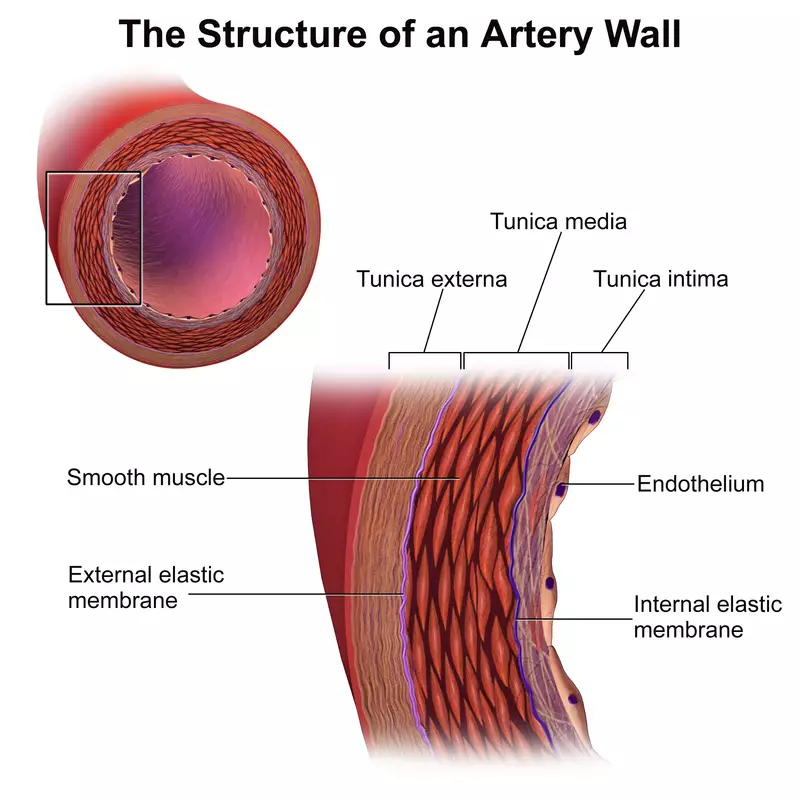
The changes in the wall of the artery occur in a process which is outlined step-by-step here.
Infinite Insults:
There are over 400 known “insults” to the cardiovascular system. These are things like hyperlipidemia, inflammation, acute and chronic infections, elevated homocysteine, elevated ferritin, heavy metals, poor diet, and the list goes on. Your body recognizes these insults as a threat and mounts a response or defense against them. However, there are only 3 ways the body can respond to the multitude of insults.
3 Finite Responses:
The body recognizes the insult or attack and mounts a response in one of three ways: Inflammation, Oxidative Stress, and Vascular Immune Function. While these are 3 separate responses, they are all linked and activation of one of them usually also stimulates the other two.
The body also has what is called “metabolic memory.” It means that when it sees a particular “insult” a second time it is better at fighting it off. The response is usually more robust. When these insults occur over and over again the response can be quite dramatic.
Step 1: Endothelial Dysfunction
The very first thing that happens is endothelial dysfunction. You cannot have a cardiovascular disease without it.
Endothelial dysfunction precedes hypertension and cardiovascular disease by decades. These abnormalities will be present many years before the blood pressure starts going up. The processes that cause, or contribute to, endothelial dysfunction will filter through to the next layer of the artery, the media. This is where the vascular smooth muscle cells live.
The cool thing is that we can actually measure your endothelial function. Because we can measure it, we can also fix it. Endothelix or EndoPAT are excellent tests to measure your endothelial function.
Simvastatin combined with losartan improves endothelial function and reduces inflammatory markers to a greater extent than monotherapy with either drug in hypercholesterolemic, hypertensive patients.3 This concept supports the hypothesis that Angiotensin-I Receptor (ATr1) blockade has beneficial effects on superoxide production and nitric oxide bioavailability above that of other classes of anti-hypertensive agents. Reduced expression of components of the NAD(P)H oxidase may contribute to these effects.4
Step 2: Vascular Remodeling
The next step is arterial remodeling. Arterial remodeling occurs through inflammation, fibrosis, growth, and apoptosis which occur due to the hypertension. These are processes which are trying to protect the artery. However, over time, the process gets more robust and the artery itself starts to be negatively affected. Basically, it is an innocent bystander that gets caught in the cross-fire.
Inflammation triggers fibrosis in hypertension and cardiovascular disease. Fibrosis occurs through an increase in collagen, fibronectin and other extracellular matrix components in the arterial wall. Fibrosis is an important component of the extracellular matrix remodeling that occurs during hypertension.
Apoptosis, programmed cell death, helps to counter cell proliferation and helps adjust developmental growth. Apoptosis can be both increased and decreased in hypertension based on different tissues (including blood vessels).
These mechanisms result in remodeling of arteries and arterioles. These mechanisms are initially adaptive and protective to prevent blow out as previously mentioned. However, when these processes continue they become maladaptive and contribute to many of the negative effects associated with hypertension.
These ‘adaptive’ mechanisms are working to protect the fragile capillaries from excess pressure. The pre-capillary resistance arterioles begin contracting in order to try to reduce blood flow and pressure within the capillary. Unfortunately, this can result in a mismatch between the amount of oxygen required by the tissues being supplied by that capillary bed and the amount of blood flow (oxygen supply) to those tissues. This can result in local tissue ischemia.10
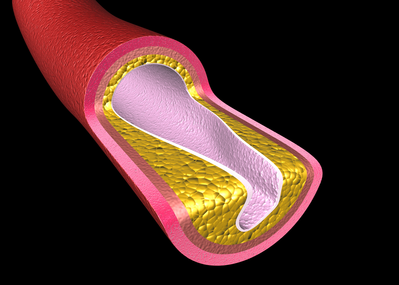
Step 3: Media/Lumen Ratio
Because of the vascular remodeling, the media (where the vascular smooth muscle cells live) gets thicker. It becomes hyper-responsive to chemicals such as catecholamines and cortisol so a little stimulation by these causes substantial vasoconstriction. This results in an exaggerated response to even small stimuli.
When arteries are exposed to increased pressures chronically, as in hypertension, they undergo changes. These changes can either be inward eutrophic remodeling or hypertrophic remodeling.1
Inward eutrophic remodeling the artery lumen, as well as the outer wall diameter, are decreased. The media/lumen ratio is increased and the media cross-section remains the same. Basically, the artery wall gets thicker and grows inward into the lumen. This type of remodeling is more common in mild essential hypertension. Hypertrophic remodeling is where the media gets thicker and begins to move in to the lumen. This results in an increase in the media cross-sectional area and the media/lumen ratio. This form is more common in severe hypertension.
Step 4: Vascular Wall Thickness Increases
The wall of the artery gets thicker.
The process begins with the small resistance and pre-capillary arteries. These arteries are very small (less than 100 μm in size. These small arteries respond to the increased wall tensile stress (increased blood pressure) with eutrophic remodeling moving into the lumen without the artery itself getting larger externally.10
This inward growth constricts the lumen and reduces blood flow and may contribute to ischemia. At the same time, the muscle in the wall of the artery is getting bigger so when it constricts it really clamps down and can stop blood flow altogether. Now you have complete occlusion of the artery.
This is what is happening in the brain when there is “white matter disease.” These are micro-infarcts in the brain due to the intense myogenic response and eutrophic remodeling due to the underlying vasculopathy. Basically, the lack of blood flow into these areas results in a very small infarct or stroke. However, they are so small that they don’t really get noticed by the patient nor the doctor clinically.
This process also occurs in the peripheral circulation but it is noticed less frequently. These patients will often complain of foot pain or tingling and they are told they have neuropathy. That is true. However, the underlying problem is the hypertension and vasculopathy causing vasoconstriction of the small arteries that supply the nerves. You then get small infarcts in the nerve resulting in neuropathy.
The larger arterioles (100-300 μm in size) have less myogenic constrictive response but they still undergo some of the same other changes. These tend to be affected later on, after the small arteries.
Although it is recognized that the cause of hypertension can be various, once blood pressure has become established structural changes emerge in the systemic vasculature. In medium- and large-sized vessels, as in the left ventricle, there is clear histological evidence of hypertrophy of the medial smooth muscle layers but, downstream in small arteries, which modulate vascular resistance, other changes occur. In essential hypertension, the smooth muscle cells of small vessels are restructured around a smaller lumen, but there is no evidence of hypertrophy or hyperplasia of the vascular wall. In secondary forms of hypertension, which tend to be representative of severer forms of the disease, hypertrophic remodelling is observed. Similarly, in non-insulin-dependent diabetes mellitus, irrespective of whether blood pressure accompanies this disorder or not, hypertrophy is also seen. The presence of architectural alterations in the vascular wall of small arteries may have a strong prognostic significance in patients, and this may be over and above all other known cardiovascular risk factors. Although it is yet to be established whether regression of such changes should be a goal of effective antihypertensive therapy, there is a body of evidence emerging indicating that different classes of antihypertensive drug have a varied effect on reversing vascular structure both in humans and animal models of genetic and experimental hypertension. However, at present, there are no data available concerning the prognostic impact of regressing vascular structural alterations in hypertension, and this must be an urgent research priority.8 .
Step 5: Arterial Compliance Decreases
With all of these changes, the artery wall becomes thicker and stiffer. It can’t expand like it could previously and compliance decreases. These changes are more profound and are first evident in the small arteries. Over time, it will also affect the large arteries. We can measure the arterial compliance and elasticity with the CV Profile and the DPA.
CCBs, ACEi, and ARBs improve arterial compliance but BBs didn’t.5
Nifedipine treatment diminished the number of severe clinical outcomes in elderly hypertensives significantly.6
Step 6: Systemic Vascular Resistance
Step 7: Hypertension
The change in small artery morphology caused by perindopril was not accompanied by any change in media cross-sectional area, suggesting that the change was due to “remodeling.”7 .
Thus, hypertensive patients with blood pressure controlled with the combination per/ind had normalized capillary density and endothelial function, whereas other antihypertensive treatments, excluding ACE inhibitors or diuretics, had less effect despite similar blood pressure control.9 .
References
- Schiffrin E, Intengan H. Vascular Remodeling in Hypertension, Roles of Apoptosis, Inflammation, and Fibrosis. Hypertension. 2001;38:581–587.
- Young RH, Ding YA, Lee YM, Yen MH. Cilazapril reverses endothelium-dependent vasodilator response to acetylcholine in mesenteric artery from spontaneously hypertensive rats. Am J Hypertens. 1995 Sep;8(9):928-33.
- Kon Koh K, Michael J. Quon M, Hwan Han S, Chung W, Yeal Ahn J, Seo Y, Ho Kang M, Hoon Ahn T, Suck Choi I, Kyun Shin E. Additive Beneficial Effects of Losartan Combined With Simvastatin in the Treatment of Hypercholesterolemic, Hypertensive Patients. Circulation. 2004;110:3687–3692.
- Brosnan MJ1, Hamilton CA, Graham D, Lygate CA, Jardine E, Dominiczak AF. Irbesartan lowers superoxide levels and increases nitric oxide bioavailability in blood vessels from spontaneously hypertensive stroke-prone rats. J Hypertens. 2002 Feb;20(2):281-6.
- Resnick L, Lester M. Differential effects of antihypertensive drug therapy on arterial compliance. Am J of Hypertension. 2002 Dec;15(12):1096-1100.
- Gong L, Zhang W, Zhu Y, Zhu J, Kong D, Pagé V, Ghadirian P, LeLorier J, Hamet P. Shanghai trial of nifedipine in the elderly (STONE). J Hypertens. 1996 Oct;14(10):1237-45.
- Thybo NK, Stephens N, Cooper A, Aalkjaer C, Heagerty AM, Mulvany MJ. Effect of antihypertensive treatment on small arteries of patients with previously untreated essential hypertension. Hypertension. 1995 Apr;25(4 Pt 1):474-81.
- Agabiti-Rosei E, Heagerty AM, Rizzoni D. Effects of antihypertensive treatment on small artery remodelling. J Hypertens. 2009 Jun;27(6):1107-14.
- Debbabi H, Bonnin P, Levy BI. Effects of blood pressure control with perindopril/indapamide on the microcirculation in hypertensive patients. Am J Hypertens. 2010 Oct;23(10):1136-43.
- Yannoutsos A, Levy BI, Safar ME, Slama G, Blacher J. Pathophysiology of hypertension: interactions between macro and microvascular alterations through endothelial dysfunction. J Hypertens. 2014 Feb;32(2):216-24. doi: 10.1097/HJH.0000000000000021.