CV Profiler (CAPWA)
The CV Profiler is also known as the Computerized Arterial Pulse Wave Analyzer (CAPWA). This device measures arterial elasticity in a cost-effective, non-invasive measure. Arterial elasticity is one of the initial events in cardiovascular disease.
There are hundreds of known risk factors for cardiovascular disease. In response to these insults, the body responds with what are known as the 3 finite responses (inflammation, oxidation, vascular immune function).7
These 3 finite responses result in endothelial dysfunction followed by decreased arterial elasticity. Endothelial function can be measured with either the EndoPAT or Endothelix devices. Arterial elasticity is accurately measured with the CV Profiler.
Why Get The CV Profiler Test?
I can tell you why I got this test. I don’t ever want to have a heart attack! This test has a few benefits:
- The earliest heart disease identification available
- Fast, non-invasive, and very cost-effective (affordable)
- Information on vascular disease is backed by numerous scientific studies
Cardiovascular disease is the #1 cause of death for men and women. The incidence of cardiovascular disease is getting worse and costs are skyrocketing. The scary thing is that we have reached a plateau in our ability to identify who will have a heart attack. For all of our efforts, we only identify 50%. One half of all people having a heart attack were not identified by traditional medical evaluations. That is why we see so many people having heart attacks who have had all of the appropriate tests (blood pressure, blood sugar, cholesterol, etc) and cleared by traditional standards.
50% of patients having a heart attack have normal cholesterol levels. 50% of heart attack victims have normal blood pressure.
Many patients who are having a heart attack have no idea they have cardiovascular disease.
You may be wondering, if the traditional approach can’t find cardiovascular disease, how do you know if you have it or you don’t?
That is exactly what we aim to do at our Tulsa Integrative Medicine clinic and we do it by understanding how cardiovascular disease begins and comprehensively testing the risk factors as well as vascular function and structure. The CV Profiler tests the vascular structure and function and is an excellent screening test for cardiovascular disease.
The CV Profiler shows you if you have cardiovascular disease at one of its earliest stages. Finding it early enables us to formulate a treatment plan to REVERSE the processes causing cardiovascular disease. After starting a treatment plan, repeating the CV Profiler test allows you to see if the treatment plan is working.
Other tests for cardiovascular disease (ultrasound, MRI, CT Scans, X-rays, blood tests, executive screenings, and stress tests) can only detect heart disease when there is already plaque in the artery. The CV Profiler is actually measuring artery disease markers and not risk factors making it much more specific for your cardiovascular disease.
The CV Profiler, in conjunction with other comprehensive cardiovascular tests, is an essential component of a preventive cardiology so that you don’t have heart attack like 1/3 of Americans.
How Is The Test Performed?
This test is done quickly and painlessly in our clinic. We are one of the only clinics (if not the ONLY clinic) with this testing capability.
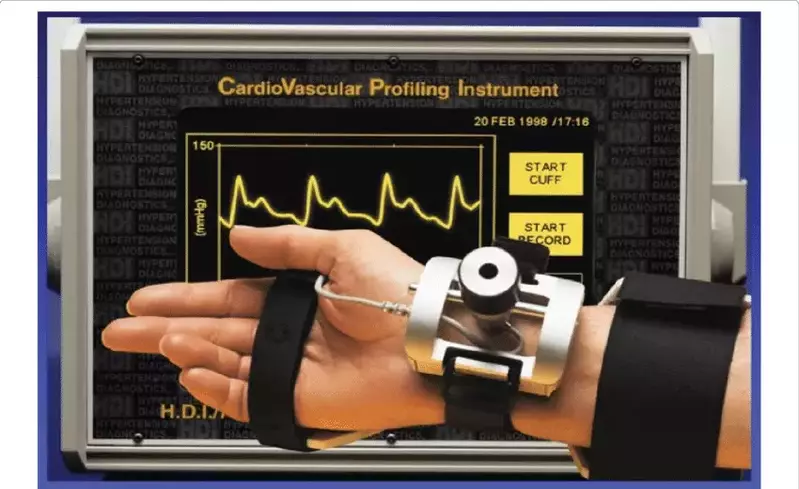
You will be taken to the testing room laid down on the exam table. A blood pressure cuff is placed on your left arm and the pulse wave analyzer (depicted in the image above) is placed on your right wrist. The analyzer will be adjusted to fine tune the pulse wave for the analysis. The test starts with a blood pressure check followed by analysis of your radial artery pulse wave. You simply have to lay still for a couple of minutes and the test will be completed.
I’ve done this test several times on myself and it is quick and painless.
How To Read The Report:
The report provides a fair amount of information: Systolic and Diastolic blood pressure, pulse pressure, mean arterial pressure, pulse rate, C1 Elasticity Index, and C2 Elasticity Index. All of this information is resulted on the first page.
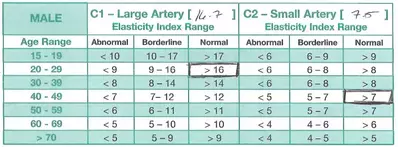
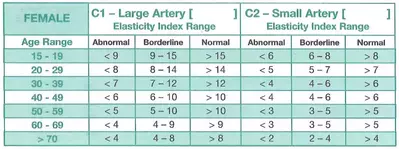
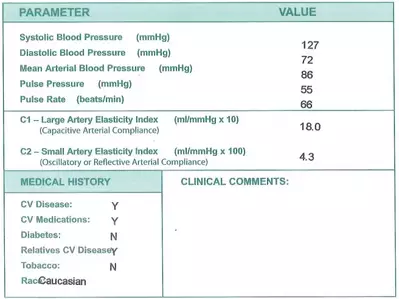 The C1 and C2 Elasticity Index provides excellent information but needs to be interpreted. There is a male and female table to enable interpretation. These tables have a column for Abnormal, Borderline, and Normal for both C1 and C2.
The C1 and C2 Elasticity Index provides excellent information but needs to be interpreted. There is a male and female table to enable interpretation. These tables have a column for Abnormal, Borderline, and Normal for both C1 and C2.
Write down the C1 & C2 Elasticity Index in the box available. Using the patient’s age, determine if the score is Abnormal, Borderline, or Normal. For the patient below, their C2 index would be Borderline for a 20-29 year old male but is Normal for a 40-49 year old male.
How Does the CV Profiler Get Its Information?
The CV Profiler is analyzing the arterial pulse wave to assess arterial stiffness. Stiff arteries are sick arteries. Young, elastic arteries suggest good vascular health. The basis for the information is below.
There are 3 types of arteries:
- Conduit (capacitive): C1. Conduit arteries store blood in systole and buffer the pressure. They have a thin endothelium with thick layers of elastin and collagen. There is less vascular smooth muscle in these arteries.
- Branch (oscillatory): C2. Pressure oscillations & reflected waves. They consist of intermediate structures.
- Arterioles (Resistance): C2. These arteries control blood flow. They are primarily composed of vascular smooth muscle and endothelium with minimal elastin or collagen. They are Nitric Oxide dependent and an early marker of vascular disease (hypertension, hyperlipidemia, and diabetes). The role of the endothelium is greatest in thin wall vessels (oscillatory and resistance). Endothelial dysfunction occurs earliest and has the greatest effect in C2 vessels.
Arterial Elasticity and Buffering Capacity
Arteries have a “buffering capacity” where they expand during systole but then constrict during diastole. The heart pumps blood in 2 phases termed systole (when the heart ventricles are squeezing) and diastole (when the ventricles are relaxing). If the arteries were solid (like a steel pipe) then the 2 phases of heart pumping would result in a very pulsatile blood flow where blood only flows during a small portion of the cycle. Elastic arteries help maintain a more constant blood flow. Compliant (elastic) arteries have good buffering capacity.
During systole (when the ventricles of the heart are contracting or squeezing) there is a rapid infusion of blood into the aorta from the stroke volume being pumped out from the heart. 20-30% of the blood coming out of the heart is forward flow and 70-80% is stored in the large conduit (capacitive) arteries temporarily. The stored blood is then released during diastole when the heart is relaxing. This buffering capacity converts the pulsatile flow in the aorta to a more continuous flow in the capillaries (Windkessel effect) and is essential for arterial health.
Stiff arteries lose this buffering capacity. The loss of buffering that occurs with decreased arterial compliance reduces continuous flow but increases pulsatile flow to pre-capillary and capillary vasculature. The increased pulsatile flow induces small vessel damage, end organ dysfunction, and end organ damage.
This results in increased systolic blood pressure, decreased diastolic blood pressure, increased pulse pressure, left ventricular hypertrophy, and increased pressure transmission to the smaller arteries resulting in arteriolar damage. Decreased arterial compliance causes an out of phase propagation of flow and pressure waves which are faster and more distorted. There is also a reflected wave resulting in an augmented pressure (augmentation index).
Noninvasive applanation tonometry – computerized arterial pulse waveform analysis (CAPWA)
- synthesize arterial pulse waveform analysis
- central hemodynamics improves: diagnosis, monitoring, prognosis
- index of wave augmentation: arterial stiffness, vascular load, wave reflection, coronary perfusion
- evaluated therapy central vs peripheral pressure discrepancies
- increased pulse wave velocity correlates with increased 24 hour heart, especially after 50 years of age
- pulse wave velocity is an independent risk factor for cardiovascular disease in hypertension
Loss of Elasticity is a Marker for Atherosclerotic Plaque Burden. Elasticity measurements can be used for identification of patients with diffuse atherosclerotic processes of the coronary arteries. Small Artery Elasticity was found to be an independent predictor of coronary artery status as assessed by angiogram.2 .
Loss of Small Artery Elasticity is Predictive of Cardiovascular Events. For every 2-unit decrease in C2-Small Artery Elasticity Index, there is a 50% increase in cardiovascular events (p < .001). Overall accuracy of C2-Small Artery Elasticity in predicting likelihood of cardiac events = 76.8%. Occurrence of events as a function of baselinearterial compliance: N=419 subjects, 1 to 7 year follow-up; End points: MI, stroke, TIA, angina, coronary or peripheral revascularization, coronary artery or peripheral bypass graft, death.3 .
Repeatability of Arterial Elasticity Assessments: Healthy subjects from 7 European sites. Intra-visit measurements taken 5 minutes apart differed by less than 3%. Inter-visit measurements taken 1-5 weeks later differed by less than 4%. Conclusion: Measurement of AE is highly reproducible despite the fact that BP and hemodynamic status was not identical.4
Small Artery Elasticity is a Sensitive Marker for Endothelial Dysfunction5
1 – Measured using high-fidelity echo-tracking ultrasound
2 – Measured using HD’s CardioVascular Profiling System
American Society of Hypertension Emphasizing Need to Go Beyond Blood Pressure.6 2005 definition of hypertension from ASH:
– Vascular abnormalities are central to the identification and treatment of hypertension
– Need to identify where the patient is on the disease continuum to individualize assessment and treatment
– Need global cardiovascular disease risk assessment, need to go beyond lowering blood pressure
2007 ESH guidelines for treating hypertension now include vascular assessment
Who Should Get The CV Profiler Test?
Male or females between the ages of 15 to 65 that have at least one risk factor of cardiovascular disease:
- family history of CV disease
- family history of obesity
- family history of diabetes
- smokers
- family history of elevated cholesterol
- sedentary lifestyle
- family history of high blood pressure
References
Schiffrin E, Intengan H. Vascular Remodeling in Hypertension – Roles of Apoptosis, Inflammation, and Fibrosis. Hypertension. 2001;38:581–587. https://doi.org/10.1161/hy09t1.096249
Syeda, B. et al, Arterial Compliance: A Diagnostic Marker for Atherosclerotic Plaque Burden?, American Journal of Hypertension, 16:356-362, 2003, ( U of Vienna, Austria) Ref: 197
Grey, E. et.al, Small But Not Large Artery Compliance Predicts Cardiovascular Events, American Journal of Hypertension 16(No. 4), 265-269, 2003, (U of MN) Ref: 172
Zimlichman, R. et. al, Determination of Arterial Compliance Using Blood Pressure WaveformAnalysis with the CR-2000 System, American Journal of Hypertension 18 (No.1):65-71, 2005
Gilani, M et al., Role of nitric oxide deficiency and its detection as a risk factor in prehypertension, Journal of the American Society of Hypertension 1(No. 1), 45-55, 2007; Ref 261
Giles, T. et.al, Expanding the Definition and Classification of Hypertension, The Journal of Clinical Hypertension 7 (No. 9):505-512, Ref. 229A
Mark C. Houston. Alternative and Complementary Therapies. Aug 2019.181-193.http://doi.org/10.1089/act.2019.29233.mho