A functional medicine approach to hypertension requires a thorough evaluation and understanding all of the options for therapy.
A functional medicine approach to hypertension requires a thorough evaluation and understanding all of the options for therapy.
Hypertension is the #1 contributor to cardiovascular disease.
Hypertension increases risk of heart attacks and strokes. It increases risk for kidney disease. Hypertension is a major problem!
Over 80 million people have hypertension. 25% of the US population (50 million people) have blood pressure >140/90. 50% (100 million people) have blood pressure above 120/80.
According to the National Health & Nutrition Examination Survey (NHANES IV) 31% of patients with hypertension have blood pressure controlled to less than 140/90. NHANES V was only slight better at 50.1%.1
Hypertensive patients with “adequate pharmacologic blood pressure control” on hydrochlorothiazide (HCTZ) and Beta Blockers still have substantially higher risk for cardiovascular morbidity and mortality – 30% greater than their normotensive counterparts.2-4
Hypertension is the #1 reason for prescription drugs and visits to physicians. Prescription sales in 2004 were $10 billion and in 2010 they were $20 billion.5-6 This is major big pharma business!
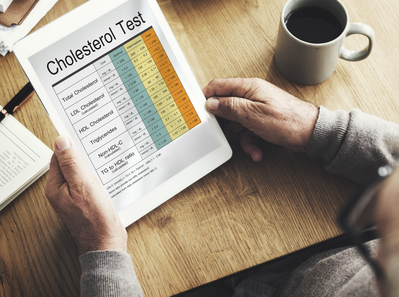
For years, we defined hypertension as a blood pressure of >140/>90. However, the Joint National Committee on Hypertension (JNC VII), published in 2003, clearly showed that risk for cardiovascular disease started at much lower levels.
It stated that increased risk for cardiovascular disease began with a systolic blood pressure of 115 and a diastolic blood pressure of 75. Risk started to increase for every point above that. In fact, risk for cardiovascular disease doubles for every 20 point increase in blood pressure over 115 and every 10 point increase in diastolic blood pressure over 75.
So, if your blood pressure is 135/75 you have double the risk of cardiovascular disease compared to someone with a blood pressure of 115/75. If your blood pressure is 155/75 then your risk is quadrupled – 400% increased risk.
2017 ACC/AHA Guidelines
In 2017, the American College of Cardiology & American Heart Association (ACC/AHA) came out with an update to JNC VII. These guidelines defined hypertension more aggressively than previous.
Blood pressure definitions:
- Normal: <120/<80
- Elevated Blood Pressure: 120-129/<80
- Hypertension, Stage 1: 130-139/80-89
- Hypertension Stage 2: 140/90 or higher
Hypertension: Systolic vs. Diastolic
Systolic blood pressure is the pressure in your artery when the ventricle (the major pumping muscle/chamber in your heart) contracts. Blood is forced through the aortic valve in the heart and the surge of blood being pumped out increases pressure in the arteries. Systolic blood pressure is the best predictor of cardiovascular disease after the age of 50.
Compliant arteries stretch to accommodate the increased blood and pressure. Stiffer arteries are unable to stretch as much and pressure increases to a greater extent.
Diastolic blood pressure is the pressure in the artery when the ventricle is relaxed. Before age 50 the diastolic blood pressure is the best predictor of risk of cardiovascular disease.
Blood Pressure Goal:
The SPRINT trial consisted of 9300 patients in 100 centers across the US since 2009. They utilitzed aggressive treatment with 2-3 medications.
they discovered that lowering blood pressure to <120 (vs 140) in patients over 50 years of age significantly reduces rates of cardiovascular disease (heart attacks, strokes, CHF, etc) by 33% and cardiovascular mortality by 25%.
Hypertension is not simply a disease of the blood pressure cuff. In fact, it is not a disease at all.
“It is the correct but chronic dysregulated response with an exaggerated outcome of the infinite insults to the blood vessel with the subsequent environmental gene expression patterns in which the vascular system is the innocent bystander. This is the maladaptive response.” Mark Houston, MD
Hypertension lets you know that the blood vessels are unhealthy and a problem is brewing. As stated above, hypertension is the #1 contributor to cardiovascular disease and we must get high blood pressure under control.
How To APPROPRIATELY Evaluate Blood Pressure:
1) Check Central Blood Pressure (Sphygmacor) – central blood pressure is MUCH better at predicting risk of target organ damage associated with elevated blood pressure.
2) 24-hour ambulatory blood pressure monitor (ABPM) evaluation. This is a blood pressure device (available in at Revolution Health & Wellness) that basically checks your blood pressure, even while you sleep. This is the GOLD STANDARD for evaluating blood pressure. In fact, you simply can’t manage blood pressure effectively and appropriately without it!
Make sure that you’ve had an appropriate blood pressure evaluation. It is very RARE that a doctor’s office checks blood pressure correctly from what I’ve seen. There are criteria for how blood pressure should be checked and most doctors aren’t doing it correctly.
3) Check Plasma Renin Activity & Aldosterone – these are blood tests that can be run through any reference lab. They tell us more about your physiology and why your blood pressure is elevated. They also change our therapy depending on the results.
4) Get a CardiaX genetic test – you only need this one once in your life. It may be critical in appropriately understanding and treating your blood pressure
How do we treat hypertension?
A lot of our therapy decisions will be based on your CardiaX results which is part of the reason why everyone with hypertension should get this lab. It may change which diet, supplements, and/or medications are recommended.
Hypertension is categorized into 2 categories based on their physiologic reason for hypertension: Low-Renin Hypertension (LRH) and High-Renin Hypertension (HRH). We treat them differently because they have different physiologic reasons for their hypertension.
Lifestyle:
- 12-hr fast every day – for example, only eat from 7am to 7pm.
- 12.5% calorie restriction. Basically, take your weight in pounds and multiply it by 10. That is your calories per day. Then take away 12.5%.
- 12.5% calorie deficit by exercise – ensure that you burn as many calories as you are restricting in your diet.
- Exercise – Resistance training for 40 minutes (high-intensity, interval type training) and 20 minutes of aerobics every day. That is a total of 60 minutes every day.
- Reduce inflammation and oxidative stress.
- Ensure that you get Olive Oil 4 tablespoons daily
- DASH-2 or Traditional Mediterranean Diet (TMD)
- Get 8 hours of sleep nightly
Supplements
There are several options for supplements to help control hypertension and decrease blood pressure.
- Magnesium – 1000mg per day in divided doses.
- Kyolic Garlic
- CoQ10
- NOmax ER –
- VitalVasc
- Neo40 Professional –
References:
- JAMA 2010;303:2043
- Current Atherosclerosis Reports 2000;2:521-8
- Hypertension 1995;25:305-13
- J Hypertension 1986;4:141-56
- Comp Health Pract Review 2000;6:11-19
- Current Atherosclerosis Report 2000;2:521-8
- https://www.nih.gov/news-events/news-releases/landmark-nih-study-shows-intensive-blood-pressure-management-may-save-lives
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014 Dec;32(12):2285-95. doi: 10.1097/HJH.0000000000000378.