Do you have low back pain or neck pain and been told that your pain is due to a herniated disk? Have you been told that surgery is your only option for treating your pain?
We have news for you… there may be another option that you may not have heard of before!
Prolotherapy can improve function and decrease back pain associated with herniated disk disease in many cases.
In order to understand how prolotherapy can help this problem we have to understand the problem itself. The spinal column is composed of 7 cervical vertebrae, 12 thoracic vertebrae, 5 lumbar vertebrae, 5 sacral vertebrae (fused), and the coccyx. There is a bony joint called the facet which connects one vertebrae to the one below. There are 2 facets per segment. These joints are held together by ligaments that form the joint capsule.
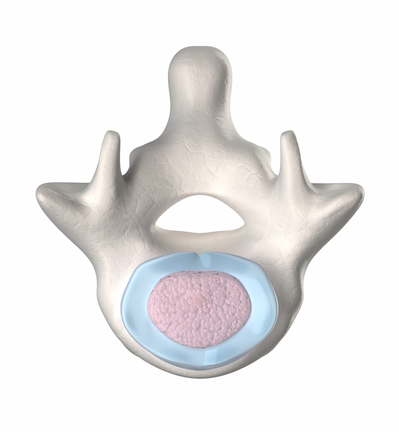
In between these vertebral segments is an inter-vertebral disk. The disk is composed of a tough outer ‘shell’ made of collagen called the annulus fibrosis. Within the outer shell is the ‘jelly filled center’ called the nucleus pulposus. The disk serves as a shock absorber and cushion.
 This structure is perfectly designed to provide structure, function, and flexibility to the human form. It allows flexion, extension, side-bending, and rotation. It is incredibly strong.
This structure is perfectly designed to provide structure, function, and flexibility to the human form. It allows flexion, extension, side-bending, and rotation. It is incredibly strong.
The weakest spot of the disk is the back side. There is a tough ligament, the posterior longitudinal ligament, that covers much of the posterior portion of the disk leaving the posterior corners the most vulnerable and this is exactly where disk herniation generally occurs.
Additionally, the spinal nerves leave the spinal canal through the intervertebral foramen. The weak spot of the disk generally corresponds to the area where this nerve exits the foramen and can compress it resulting in ‘radiculopathy’. Surgery for herniated disks involves surgically repairing the disk and decompressing the nerve resulting is elimination of radiculopathy.
One source states that the surgery SHOULD be 95% effective in eliminating the radiculopathy. However, they also state that 10% of patients will have a recurrence in the same area and require repeat surgery. They recommend a spinal fusion if this occurs repetitively.
I have a few issues with this approach.
First, not all “pain going down my leg” is due to a herniated disk, even if you find a herniated disk on MRI. Several studies have been performed that raise questions on whether or not we can accurately attribute an abnormal finding on MRI to the cause of the symptoms. Back pain should be evaluated by a trained prolotherapist before any surgery is considered (unless it is a true emergency) because there are other potential causes for pain going down the leg besides herniated disks.
Next, we need to evaluate the actual cause of the herniated disk. Have you ever wondered WHY these things occur in the first place? I don’t believe they ‘just happen’. Here’s how I believe these things get started…
Step 1: There is damage to the ligaments that form the facet joint capsule allowing excess movement and flexion.
Step 2: Excess flexion causes increased stress on the disk but also increases the stress exponentially on the anterior column (the front edge of the disk) and forces pressure posteriorly along the weakest area of the disk. This allows the disk herniation.
If I am right, we can help this problem with prolotherapy on the spinal facets which will tighten up these joints, restore proper spinal function, and provide an environment for the disk to heal itself.
We have helped many patients with herniated disks with prolotherapy!
Here is an example.
A 53 year old active duty Marine Corps Master Gunnery Sergeant with a history of repetitive low back pain after a sports injury 10 years prior. He was told that he had disk rupture with stenosis and surgery was recommended. He underwent 1 year of physical therapy and other conservative therapies and had no improvement and his left leg started hurting. He stated that his pain was getting worse and it hurt to sit and lay down.
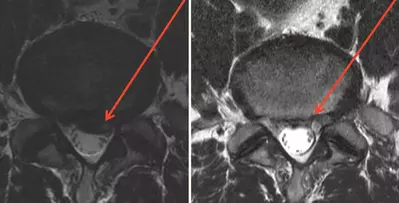
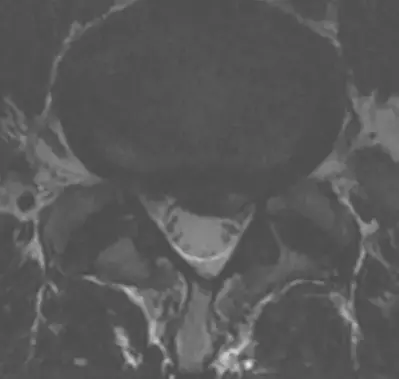
An MRI was obtained and is shown below:

June 14, 2010 – the patient received his 1st prolotherapy procedure with standard proliferant solution.
July 30, 2010 – the patients states that he has no back pain but does have some left buttock and radiating pain to the top side of his foot from 1 week prior. He received his 2nd round of prolotherapy with dextrose and added PRP at this time.
August 27 & October 2, 2010 – prolotherapy & PRP (#3 & #4). He has no back pain with only mild pain on the dorsum of his foot. He states that he is more than 90% improved at this point.
November 13, 2010 – he states he has almost no pain and he received his 5th prolotherapy procedure.
April 8, 2010 – he returned to the Army Hospital and saw his orthopedic surgeon who told him “you can’t cure ruptured disks and spinal stenosis with an injection” and that this was “nonsense!” The surgeon wanted to “prove this nonsense” with a follow up MRI.
The comparison of the before and after MRIs are below. The herniation is depicted by the arrows.
The surgeon was surprised by this MRI finding and had to admit the success. The patient stated that he had no problems with tough military training.
This case underscores the potential benefit of prolotherapy with a specific injury. We have tremendous success with treating low back pain with prolotherapy in our clinic and would love to help you with your pain.
Consider the cost of surgery: time off from work, family, and exercise; physical therapy; medications; and potential risks.
Now consider the cost of prolotherapy: no time off of work; limited recovery needed; no medications (generally); and very low risks.
The choice is clear. Contact us to schedule your prolotherapy evaluation today!