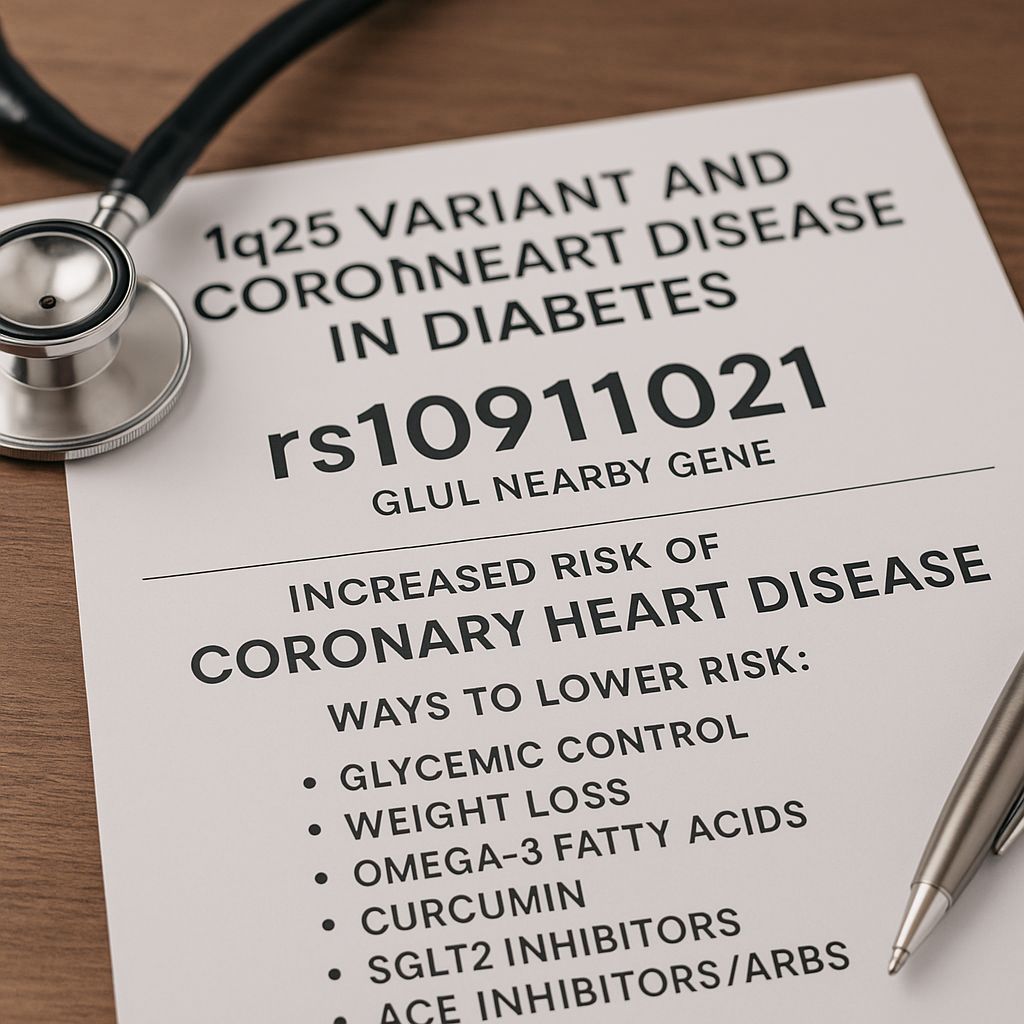
1q25 (rs10911021): A Diabetes‑Specific Coronary Heart Disease Locus—and How to Mitigate Its Risk
Cardiovascular genetics continues to uncover risk signals that traditional lipids and blood pressure cannot fully explain. One of the most clinically actionable signals for patients with type 2 diabetes (T2D) is a chromosome 1q25 variant, commonly tagged by rs10911021. Unlike many “general population” variants, 1q25 is important because its risk effect appears specific to people with diabetes and tracks with altered endothelial metabolism—pointing to concrete, modifiable pathways.
Your CardiaX report flags this locus to alert you and your clinician to a pattern of endothelial stress and redox imbalance that is especially relevant in diabetes. In this guide, you will learn what the 1q25 signal means, why it increases coronary heart disease (CHD) risk in diabetes, and how targeted nutrition, lifestyle, nutraceuticals, peptides, and medications can neutralize that risk.
Quick Facts
-
What is it? A noncoding variant at chromosome 1q25, best represented by rs10911021, located near GLUL (glutamate–ammonia ligase), which encodes glutamine synthetase. The diabetes‑specific association with CHD was first shown in multi‑cohort GWAS and replicated in independent populations.
-
What does it do? In endothelial cell models, the risk allele is associated with lower GLUL expression and disturbed glutamate ↔ glutamine handling and γ‑glutamyl cycle metabolites—metabolic hubs that regulate redox balance and nitric‑oxide bioavailability.
-
Who is most affected? Individuals with T2D; the original discovery highlighted a gene‑by‑diabetes interaction in which the 1q25 signal predicts CHD specifically in diabetes, not robustly in non‑diabetic cohorts.
-
Why it matters clinically? It points to endothelial dysfunction amenable to intervention—glycemic control, weight loss, blood pressure optimization, improved sleep, exercise, omega‑3s, magnesium, curcumin, coenzyme Q10, resveratrol, and—in the right patients—SGLT2 inhibitors, GLP‑1 receptor agonists, ACE inhibitors/ARBs, and high‑intensity statins.
Where 1q25 Lives and What It Controls
The 1q25 locus sits upstream of GLUL, a housekeeping gene that converts glutamate + ammonia → glutamine. Glutamine synthetase is crucial for:
-
Detoxifying ammonia in tissues outside the liver, including vascular endothelium.
-
Supplying glutamine to support glutathione (GSH) synthesis via the γ‑glutamyl cycle, the cell’s central antioxidant system.
-
Fueling endothelial nitric‑oxide (NO) signaling, because oxidative stress depletes NO and stiffens arteries.
In laboratory work using HUVEC (human umbilical‑vein endothelial cells), the risk allele of rs10911021 was linked to lower GLUL expression and a distinct intracellular metabolite signature within the glutamate/glutamine and γ‑glutamyl pathways. Those findings create a compelling mechanism: less GLUL → altered glutamine availability → impaired GSH recycling and redox control → endothelial dysfunction, a known driver of atherogenesis in diabetes.
Why This Variant Matters More in Diabetes
Diabetes loads the endothelium with several pro‑atherogenic hits:
-
Hyperglycemia and glycation create reactive dicarbonyls, consuming antioxidant defenses.
-
Mitochondrial over‑fueling increases ROS (reactive oxygen species).
-
Insulin resistance amplifies inflammation and reduces NO.
-
Lipotoxicity from triglyceride‑rich particles injures the vascular wall.
When a patient already has this high‑stress metabolic milieu, any genetic reduction in GLUL function or expression can tip the system toward oxidative damage, impaired NO signaling, and plaque formation. The discovery GWAS emphasized this gene‑by‑environment (diabetes) interaction, which is why CardiaX calls out 1q25 for diabetes‑associated CHD risk rather than for the general population.
Clinical Phenotypes to Watch
Patients who carry the 1q25 risk allele and have diabetes often display one or more of the following patterns:
-
Elevated fasting glucose or A1c, or significant glycemic variability.
-
Low HDL or elevated triglycerides (insulin resistance signature).
-
Markers of oxidative stress or inflammation (e.g., hs‑CRP).
-
Endothelial dysfunction signs—hypertension, impaired flow‑mediated dilation, microalbuminuria.
These features do not prove causality from the SNP, but they magnify the penetrance of the genetic signal and highlight intervention targets.
Testing Context: CardiaX and Beyond
-
CardiaX includes 1q25 among a panel of cardiovascular SNPs to personalize prevention plans. Your result flags whether you carry the risk allele and thus may benefit from a more aggressive endothelial‑centric strategy. (CardiaX is provided by Vibrant Wellness.)
-
We often pair genetic results with phenotypic testing—lipids and Lp(a), PULS (vascular injury biomarkers), insulin resistance panels, DEXA for visceral fat, and central blood pressure—to move from risk to precise action.
How to Lower Risk if You Carry 1q25
Because the 1q25 signal maps to endothelial redox and NO biology, the mitigation plan focuses on glycemic excellence, oxidative‑stress control, inflammation reduction, and hemodynamic protection.
1) Foundational Lifestyle
Nutrition
-
Emphasize a Mediterranean or low‑glycemic, fiber‑forward pattern with vegetables, legumes, nuts, extra‑virgin olive oil, and fatty fish.
-
Target 30–40 g/day of fiber; include soluble fibers (oats, psyllium) to improve post‑meal glucose and triglycerides.
-
Reduce ultra‑processed foods, refined sugars, and excess starch to ease oxidative load and glycemic swings.
-
Limit alcohol; if consumed, keep intake light and with meals.
Body Composition & Activity
-
Aim for 7–10% weight loss if overweight; even modest loss improves endothelial function.
-
Perform 150–300 minutes/week of mixed aerobic training plus 2–3 resistance sessions for insulin sensitivity and vascular shear stress benefits.
-
Incorporate zone‑2 sessions for mitochondrial efficiency; add occasional HIIT once glucose control stabilizes.
Sleep & Stress
-
Secure 7–9 hours/night; screen and treat sleep apnea.
-
Practice mindfulness, breath work, or yoga to reduce sympathetic tone that worsens endothelial stress.
2) Targeted Nutraceuticals
These support glutathione cycling, NO bioavailability, lipid quality, and inflammation control—the very nodes implicated by 1q25.
-
Omega‑3 fatty acids — Omega 1300. EPA/DHA improve endothelial function, lower triglycerides, and reduce post‑prandial inflammation.
-
Curcumin — Curcumin Complex. Curcumin downregulates NF‑κB and improves endothelial NO synthase coupling.
-
Coenzyme Q10 + Omega — CoQ10 Omega. Supports mitochondrial electron transport and reduces oxidative stress that consumes glutathione.
-
Magnesium glycinate — enhances insulin sensitivity and stabilizes vascular tone.
-
Resveratrol — supports endothelial NO and SIRT1 signaling, with favorable effects on glycemia.
-
N‑acetylcysteine (NAC) — a precursor for glutathione that can replenish GSH when γ‑glutamyl cycling is stressed.
-
Vitamin D — immune‑endothelial modulator; optimize to individualized ranges.
Why these? The HUVEC metabolomic work at 1q25 points toward glutamate/glutamine and γ‑glutamyl cycle imbalance; strategies that bolster GSH and NO directly counter that biology. (Diabetes Journals, Iris)
3) Peptides (Clinic‑Supervised)
While human cardiovascular outcome data for peptides remain limited, several options may indirectly benefit 1q25 carriers by reducing systemic inflammation, improving endothelial health, or supporting metabolic control:
-
KPV — Potent anti‑inflammatory tripeptide that down‑modulates cytokine signaling.
-
BPC‑157 — Supports microvascular integrity and accelerates tissue healing; may aid gut‑endothelial crosstalk.
-
MOTS‑c — Mitochondrial peptide that improves insulin sensitivity and metabolic flexibility; beneficial for the diabetic environment that amplifies 1q25 risk.
Peptides are for research purposes or specific indications and should be used only under physician supervision consistent with our clinic policies.
4) Medications with High‑Value Benefit
Your genotype does not prescribe a particular drug, but it tells us where to push. In T2D with CHD risk (especially in 1q25 carriers), the following classes have strong evidence:
-
SGLT2 inhibitors (empagliflozin, dapagliflozin): Reduce heart failure events and improve renal‑vascular outcomes in diabetes.
-
GLP‑1 receptor agonists (semaglutide, tirzepatide class): Lower ASCVD events, promote weight loss, and improve endothelial markers.
-
High‑intensity statins (± ezetimibe or PCSK9 if needed): Lower LDL to <55–70 mg/dL in very high‑risk patients and reduce oxidative LDL burden.
-
ACE inhibitors or ARBs: Improve endothelial function, lower BP, and protect kidneys—critical in diabetes.
-
EicosaPentanoic Acid (EPA) for patients with persistent hypertriglyceridemia: Outcome‑proven EPA therapy. This is one of the Omega-3 fatty acids.
Medication decisions remain individualized; genetics inform why we choose endothelial‑protective pathways.
Putting It Together: A Practical Protocol for 1q25 Carriers with Diabetes
-
Confirm phenotype
-
Tighten glycemic targets (e.g., A1c individualized, often ≤6.5–7.0% if safe).
-
Assess visceral adiposity (DEXA), BP (including central BP), lipids, and PULS for vascular injury.
-
-
Lifestyle reset
-
Mediterranean/low‑glycemic plan; fiber 30–40 g/day; weight loss goal 7–10%.
-
Exercise roadmap: 4–5 days/week aerobic (zone‑2 base), 2–3 days/week resistance.
-
Sleep and stress programs; screen for OSA.
-
-
Nutra‑stack (clinic‑guided)
-
Omega 1300 + CoQ10 Omega + Curcumin Complex; consider magnesium, resveratrol, NAC, and vitamin D.
-
-
Peptide consideration
-
When inflammation or metabolic inflexibility remains, consider KPV, BPC‑157, or MOTS‑c under supervision.
-
-
Pharmacologic optimization
-
Escalate to SGLT2i/GLP‑1RA, ACEi/ARB, and lipid‑lowering therapy as indicated by risk profile.
-
-
Track and adapt
-
Reassess labs, body comp, BP, and PULS at 3–6 months; repeat CardiaX only if needed for counseling or family testing.
-
Case Vignette
Patient: 58‑year‑old woman with T2D (A1c 7.9%), BMI 33, hypertension, and triglycerides 245 mg/dL. CardiaX shows 1q25 risk allele (rs10911021). She has low energy and exertional dyspnea; hs‑CRP is 3.4 mg/L. CIMT suggests early plaque.
Plan:
-
Nutrition: Mediterranean‑style with 30 g fiber/day; added protein at breakfast to blunt glucose peaks; alcohol limited to ≤3 drinks/week.
-
Activity: Step‑wise program to 180 minutes/week zone‑2 + two resistance days.
-
Supplements: Omega 1300, CoQ10 Omega, Curcumin Complex, magnesium glycinate at bedtime, NAC 600 mg bid for 12 weeks.
-
Medications: Initiate empagliflozin and semaglutide (titrated), continue ARB; add high‑intensity statin given global risk.
-
Peptide: KPV short course for systemic inflammation support (clinic‑supervised).
-
Follow‑up: At 6 months A1c 6.7%, TG 140 mg/dL, hs‑CRP 1.1 mg/L, weight −8%. Central BP improved; PULS panel shows lower inflammatory injury markers. Exercise tolerance rises markedly.
Genotype did not change which evidence‑based therapies work—it clarified why endothelial‑first strategies would help most and motivated adherence.
FAQs
Does the 1q25 variant raise LDL cholesterol?
No. The association appears independent of LDL and operates through endothelial metabolic stress. Lipids remain vital to manage, but for different reasons.
Should non‑diabetic carriers worry?
Current evidence shows the strongest signal in diabetes. That said, anyone with insulin resistance or prediabetes can share a similar metabolic environment, so the same prevention blueprint remains prudent.
Can I “turn off” this gene?
You cannot change DNA, but you can change gene expression and downstream biology—especially oxidative stress, glutathione status, and glycemic load—which appears to be the key pathway for 1q25.
The Bottom Line
The 1q25 (rs10911021) signal spotlights a diabetes‑specific route to coronary disease: endothelial redox imbalance linked to GLUL and the glutamate–glutamine–glutathione axis. That is good news because it is highly modifiable. Optimize glycemia and weight, train consistently, sleep well, and use endothelial‑centric nutrition, nutraceuticals, peptides, and medications where appropriate. Combine your CardiaX insights with PULS and advanced cardiometabolic testing to verify that your plan is lowering real vascular injury, not just moving numbers on paper.
Call to action:
Ready to translate your CardiaX results into a personalized plan that protects your arteries? Schedule a consultation with our team. We will pair your genetics with targeted labs (including PULS) and design a step‑by‑step program—nutrition, supplements, peptides, and medications—to neutralize 1q25 risk and build resilient vascular health.
Scientific References
-
Qi L, et al. Association Between a Genetic Variant Related to Glutamic Acid Metabolism and Coronary Heart Disease in Diabetic Patients. JAMA. 2013;310(8):821–828. (JAMA Network)
-
Pipino C, et al. Association of the 1q25 Diabetes‑Specific Coronary Heart Disease Locus With Altered Endothelial Glutamate Metabolism. Diabetes. 2020;69(10):2206–2217. (Diabetes Journals)
-
Diabetes Study summary/reporting on 1q25–GLUL mechanism and gene‑by‑diabetes interaction. Cardiovascular Business (news coverage of peer‑reviewed findings). (Cardiovascular Business)
-
Pipino C, et al. (full‑text PDF). Diabetes 2020 supplemental analysis of intracellular metabolites in HUVECs across rs10911021 genotypes. (Iris)
Note: We tailor supplement and peptide protocols to the individual and use physician‑supervised products only. Peptides discussed are not FDA‑approved for cardiovascular indications and are for educational purposes.