ACE I/D Polymorphism: A Key Genetic Driver of Hypertension and Cardiovascular Disease
Introduction
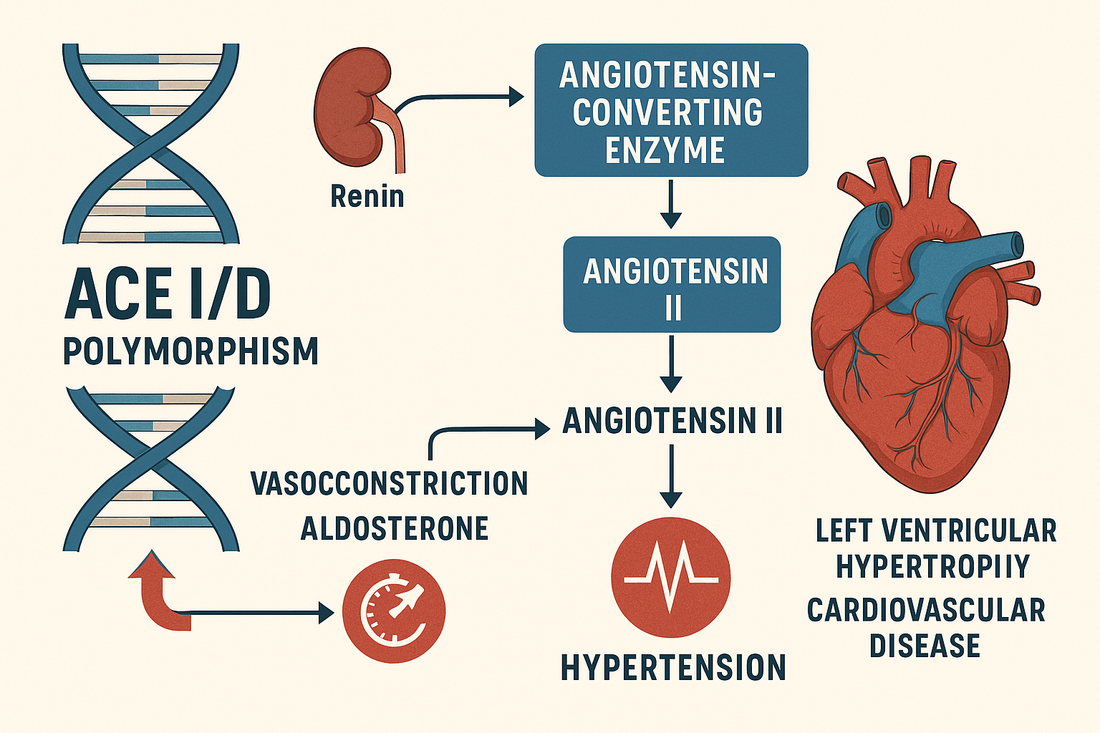
The angiotensin-converting enzyme (ACE) gene, located on chromosome 17q23, is a critical regulator of the renin–angiotensin–aldosterone system (RAAS). This system maintains blood pressure and fluid balance.
The ACE insertion/deletion (I/D) polymorphism (rs1799752)—caused by the presence (insertion, I) or absence (deletion, D) of a 287 base pair Alu repeat in intron 16—profoundly influences ACE enzyme activity:
-
DD genotype: Highest ACE activity → increased angiotensin II and blood pressure.
-
II genotype: Lowest ACE activity → reduced angiotensin II, lower BP.
-
ID genotype: Intermediate activity.
Your CardiaX test includes ACE I/D because it is strongly linked to hypertension, left ventricular hypertrophy (LVH), heart failure, myocardial infarction (MI), and stroke risk.
ACE and Cardiovascular Physiology
-
Angiotensin I → Angiotensin II conversion: ACE converts Ang I into Ang II, a potent vasoconstrictor.
-
Vascular effects: Ang II increases vascular resistance, stimulates aldosterone, and promotes sodium retention.
-
Cardiac remodeling: Ang II and aldosterone stimulate fibrosis, LVH, and vascular stiffening.
-
Inflammation: Ang II increases oxidative stress and endothelial dysfunction.
ACE I/D Polymorphism and Clinical Implications
1. Hypertension
-
DD carriers are at highest risk for essential hypertension and salt sensitivity.
-
II carriers often exhibit lower blood pressure and may have protection against hypertension.
2. Coronary Artery Disease & MI
-
D allele is associated with increased risk of myocardial infarction and earlier onset CAD.
-
Greater plaque instability and higher oxidative burden.
3. Heart Failure
-
DD genotype linked with more severe LV remodeling, hypertrophy, and worse prognosis.
4. Athletic Performance
-
D allele: Linked to power/sprint performance.
-
I allele: Associated with endurance capacity.
What Increases ACE-Driven Risk?
-
High sodium diet: Potentiates RAAS activation.
-
Obesity and insulin resistance: Increase RAAS tone and vascular inflammation.
-
Sedentary lifestyle: Reduces vascular flexibility.
-
Chronic stress: Elevates sympathetic drive, augmenting RAAS activity.
-
Low potassium intake: Favors vasoconstriction.
How to Mitigate ACE I/D-Associated Risk
1. Lifestyle Strategies
-
Low-sodium, potassium-rich diet: Emphasize leafy greens, legumes, and fruits.
-
DASH or Mediterranean diet: Both reduce BP and improve endothelial function.
-
Exercise: Aerobic + resistance training lowers RAAS activity.
-
Weight optimization: Reduces vascular inflammation and improves BP control.
-
Stress management: Meditation and yoga reduce sympathetic activation.
2. Nutraceuticals
-
Omega 1300 — Omega 1300: Lowers inflammation, reduces BP.
-
CoQ10 Omega — CoQ10 Omega: Improves endothelial function.
-
Magnesium glycinate: Promotes vasodilation and BP stability.
-
Curcumin Complex — Curcumin Complex: Anti-inflammatory and antioxidant.
-
Vitamin D3/K2: Supports vascular health and RAAS modulation.
3. Peptide Therapies
-
BPC-157: Enhances vascular healing and reduces fibrosis.
-
MOTS-c: Improves insulin sensitivity and mitochondrial efficiency.
-
KPV: Reduces systemic inflammation driven by Ang II.
4. Medications
-
ACE inhibitors (lisinopril, enalapril): Particularly effective in DD carriers with high ACE activity.
-
ARBs (losartan, valsartan): Block downstream effects of Ang II.
-
MRAs (spironolactone, eplerenone): Counteract aldosterone-mediated fibrosis.
-
Beta-blockers: Reduce sympathetic overdrive in high-risk carriers. However, it is important to stick with the newer beta-blockers (nebivolol or carvedilol).
Case Example
A 58-year-old man with DD genotype on CardiaX presents with hypertension and LVH.
Plan:
-
Lifestyle: Sodium reduction, potassium-rich Mediterranean diet, exercise.
-
Supplements: Omega 1300, CoQ10 Omega, Curcumin Complex.
-
Medications: Started on ACE inhibitor and low-dose MRA.
-
Peptides: BPC-157 considered for vascular remodeling.
Outcome: Blood pressure reduced from 158/96 to 124/78 mmHg. Echocardiogram shows regression of LVH after 12 months.
The Bottom Line
The ACE I/D polymorphism is one of the most impactful genetic variants for hypertension and cardiovascular disease risk.
-
DD carriers: Highest risk, strongest benefit from ACE inhibitors and RAAS-modulating strategies.
-
II carriers: Lower risk, endurance advantage, but still benefit from lifestyle optimization.
-
ID carriers: Intermediate phenotype, require balanced strategies.
CardiaX testing helps identify high-risk carriers and tailor interventions across diet, supplements, peptides, and medications.
References
-
Rigat B, et al. An insertion/deletion polymorphism in the ACE gene accounting for half the variance of serum enzyme levels. J Clin Invest. 1990.
-
Cambien F, et al. Deletion polymorphism in the ACE gene as a risk factor for myocardial infarction. Nature. 1992.
-
Staessen JA, et al. The insertion/deletion polymorphism of the ACE gene and cardiovascular disease. J Hypertens. 1997.
-
Schunkert H, et al. Association between a deletion polymorphism of the ACE gene and left ventricular hypertrophy. N Engl J Med. 1994.