ADRB2 Gene Variants and Cardiovascular Disease
Introduction
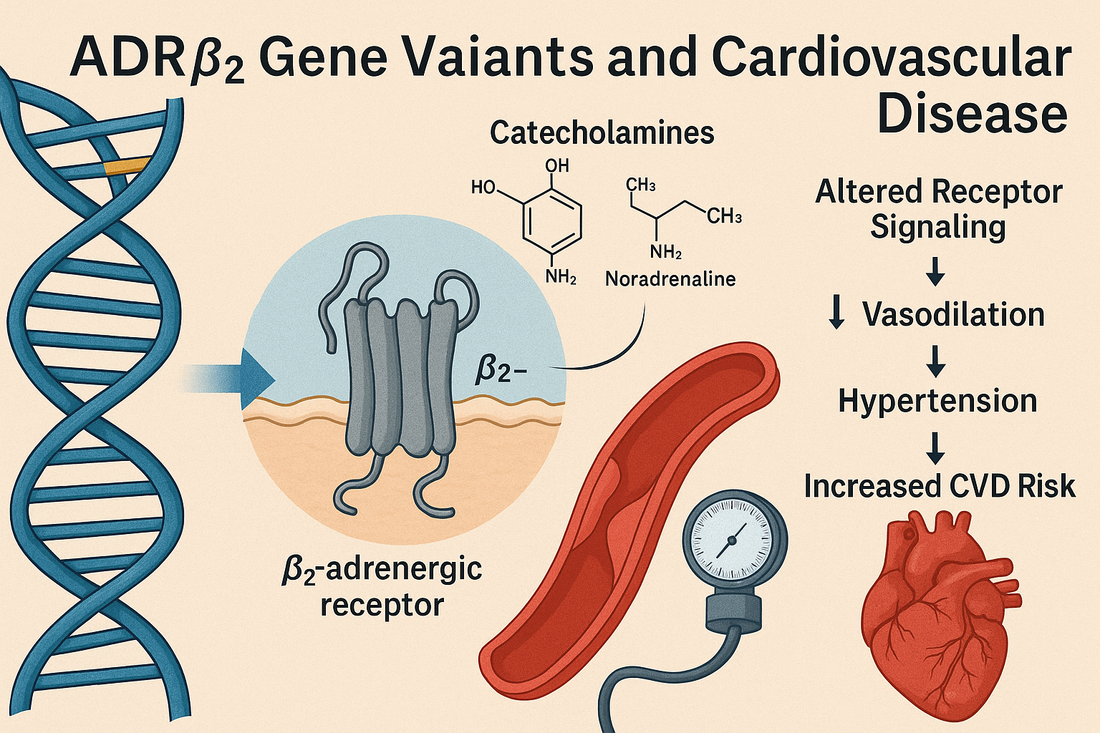
The ADRB2 gene encodes the β2-adrenergic receptor (β2-AR), a critical receptor in the sympathetic nervous system. Located on chromosome 5q31-32, this receptor regulates vascular tone, heart rate, and metabolic function by binding catecholamines (epinephrine and norepinephrine).
Variants in ADRB2 can alter receptor sensitivity and downstream signaling, affecting blood pressure regulation, endothelial function, lipid metabolism, and risk of cardiovascular disease (CVD). CardiaX testing evaluates key ADRB2 SNPs to personalize prevention strategies.
ADRB2 Function in the Body
-
Vascular regulation: Mediates smooth muscle relaxation → vasodilation and lower blood pressure.
-
Cardiac effects: Modulates heart rate and contractility.
-
Metabolic role: Influences glucose and lipid metabolism.
-
Exercise response: Determines how efficiently the body adapts to catecholamine surges during activity.
Key ADRB2 Variants
rs1042713 (Arg16Gly)
-
Gly16 allele: Associated with enhanced receptor downregulation → reduced responsiveness to catecholamines.
-
Impact: Higher risk of hypertension, altered vascular reactivity, reduced exercise-induced vasodilation.
rs1042714 (Gln27Glu)
-
Glu27 allele: Resistant to downregulation, linked to obesity, insulin resistance, and lipid abnormalities.
-
Impact: May worsen CVD risk when combined with poor lifestyle factors.
rs1800888 (Thr164Ile, rare)
-
Reduces receptor function and responsiveness. Associated with increased risk of heart failure and coronary events.
How ADRB2 Variants Contribute to Cardiovascular Risk
-
Hypertension – Altered vascular tone due to receptor downregulation or dysfunction.
-
Endothelial dysfunction – Impaired vasodilation reduces blood flow and increases arterial stiffness.
-
Atherosclerosis – Through effects on lipids, inflammation, and vascular reactivity.
-
Heart failure risk – Particularly with rare variants reducing β2-AR signaling.
-
Blunted exercise adaptation – Reduced improvement in VO₂ max and vascular flexibility in risk allele carriers.
What Worsens ADRB2-Related Risk?
-
High catecholamine states (chronic stress, untreated OSA).
-
Sedentary lifestyle (reduces compensatory vasodilation capacity).
-
High sugar and fat diets (increase insulin resistance, worsening receptor function).
-
Smoking (further impairs adrenergic signaling and vascular repair).
How to Mitigate ADRB2-Associated Risk
1. Lifestyle Strategies
-
Exercise: Aerobic and resistance training enhance adrenergic signaling efficiency and improve vascular tone.
-
Diet:
-
Mediterranean diet rich in omega-3s, fiber, and antioxidants.
-
Reduce refined carbs and added sugars to combat insulin resistance.
-
Adequate potassium and magnesium intake for vascular relaxation.
-
-
Stress management: Mind-body practices lower sympathetic overdrive.
-
Sleep hygiene: Essential for balancing catecholamine rhythms.
2. Nutraceuticals
-
Omega 1300 — Omega 1300: Improves endothelial health and lowers BP.
-
CoQ10 Omega — CoQ10 Omega: Enhances energy efficiency in cardiac muscle.
-
Curcumin Complex — Curcumin Complex: Reduces oxidative stress that impairs β2-AR signaling.
-
Magnesium: Promotes vasodilation, reduces arrhythmia risk.
-
L-arginine or citrulline: NO precursors to support vasodilation.
3. Peptides
-
MOTS-c: Improves mitochondrial efficiency and exercise response.
-
BPC-157: Supports vascular repair and endothelial function.
-
KPV: Mitigates chronic inflammation that worsens receptor function.
4. Medications
-
Beta-blockers: Response varies by ADRB2 genotype—some carriers have diminished effect. Alternatives (ACEi, ARBs, calcium channel blockers) may be better.
-
ACE inhibitors/ARBs: Support vascular relaxation and reduce hypertension.
-
Statins: Improve endothelial function independent of LDL lowering.
-
GLP-1 agonists or SGLT2 inhibitors: For carriers with metabolic syndrome or diabetes, supporting both vascular and metabolic health.
Case Example
A 45-year-old male, ADRB2 Gly16Gly genotype, presents with borderline hypertension and poor exercise tolerance. Despite HDL-C of 55 mg/dL, his central BP is elevated, and he has a family history of premature heart disease.
Plan:
-
Lifestyle: Mediterranean diet, structured exercise, stress management.
-
Supplements: Omega 1300, CoQ10 Omega, magnesium, citrulline.
-
Peptides: MOTS-c and KPV for improved vascular response.
-
Medications: Initiated ARB rather than beta-blocker due to ADRB2 variant profile.
Outcome: After 6 months, BP decreased from 142/88 to 124/76, VO₂ max improved, and inflammatory markers decreased.
The Bottom Line
The ADRB2 gene plays a pivotal role in cardiovascular regulation. Variants can reduce vascular responsiveness, increase hypertension risk, and impair exercise benefits.
By identifying ADRB2 variants through CardiaX, clinicians can personalize strategies—leveraging nutrition, exercise, supplements, peptides, and medications—to restore vascular health and lower CVD risk.
References
-
Johnson JA, et al. Beta-adrenergic receptor polymorphisms and cardiovascular disease. Pharmacogenomics J. 2006.
-
Taylor MR. β-adrenergic receptor polymorphisms and their association with CVD. Pharmacogenomics. 2007.
-
Green SA, et al. Influence of β2-adrenergic receptor polymorphisms on vascular reactivity. N Engl J Med. 1995.
-
Liggett SB, et al. Genetic polymorphisms of the β2-adrenergic receptor and cardiovascular phenotypes. J Clin Invest. 1998.