AGTR1: Gene Variants and Their Role in Cardiovascular Disease
Introduction
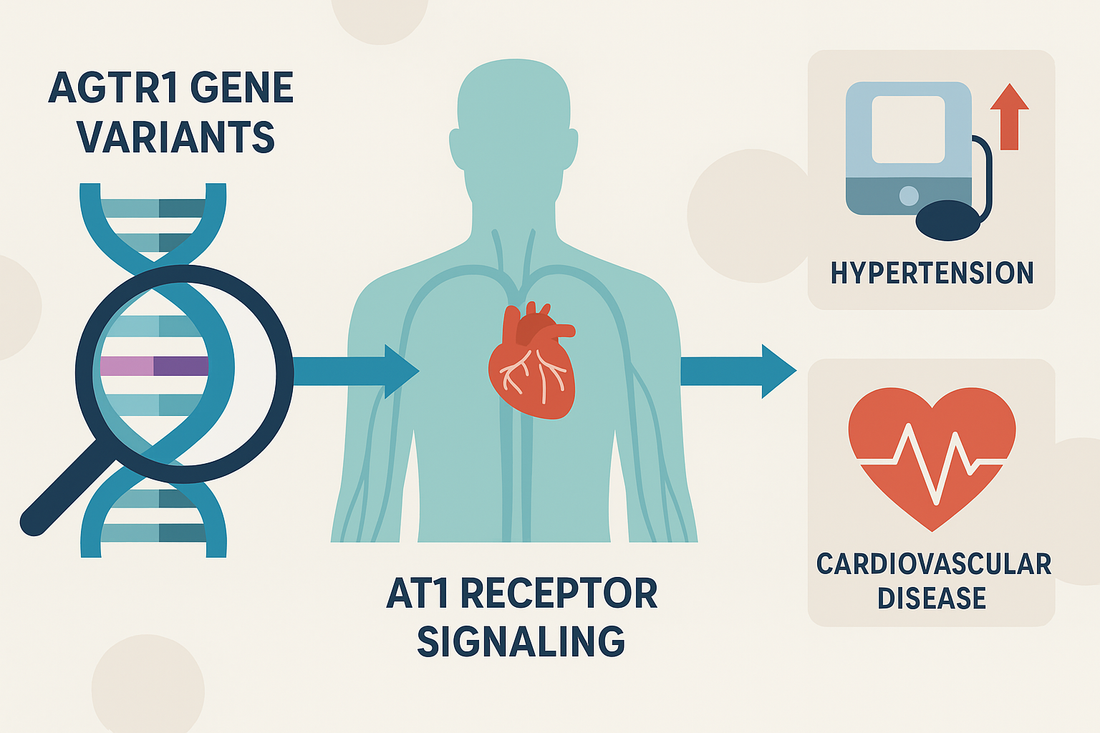
The AGTR1 gene encodes the angiotensin II type 1 receptor (AT1R), a central regulator of the renin-angiotensin-aldosterone system (RAAS). Activation of this receptor drives vasoconstriction, aldosterone release, sodium retention, and vascular remodeling.
Genetic variants in AGTR1 alter receptor activity and expression, impacting hypertension susceptibility, vascular injury, and long-term cardiovascular disease (CVD) risk. The CardiaX genetic test evaluates AGTR1 to help clinicians develop personalized cardiovascular prevention and treatment strategies.
Biological Role of AGTR1
-
Vasoconstriction: Mediates angiotensin II–induced narrowing of blood vessels.
-
Aldosterone release: Increases sodium and water retention, raising blood pressure.
-
Vascular remodeling: Promotes smooth muscle hypertrophy and fibrosis.
-
Inflammation & oxidative stress: AT1R activation stimulates NF-κB and reactive oxygen species, contributing to atherosclerosis.
Key AGTR1 Variant
A1166C (rs5186)
-
Most studied AGTR1 SNP.
-
C allele carriers: Higher receptor expression and sensitivity to angiotensin II.
-
Linked with:
-
Hypertension (especially salt-sensitive).
-
Left ventricular hypertrophy.
-
Coronary artery disease and stroke risk.
-
-
AA genotype: Lower receptor activation and more favorable cardiovascular profile.
How AGTR1 Variants Impact Cardiovascular Risk
-
Hypertension: Increased AT1R signaling elevates vascular tone and blood pressure.
-
Atherosclerosis: Chronic vascular inflammation accelerates plaque formation.
-
Endothelial dysfunction: Reduced nitric oxide availability impairs vasodilation.
-
Heart failure and remodeling: Long-term overactivation contributes to left ventricular hypertrophy and fibrosis.
Risk Factors That Amplify AGTR1-Associated Risk
-
High sodium intake
-
Obesity and insulin resistance
-
Chronic kidney disease
-
Smoking and alcohol excess
-
Sedentary lifestyle
-
Low potassium intake
How to Mitigate AGTR1-Associated Risk
1. Lifestyle Modifications
-
Diet:
-
Low-sodium, high-potassium diet (DASH or Mediterranean patterns).
-
Emphasize vegetables, fruits, legumes, fish, nuts, olive oil.
-
Reduce processed foods and added sugars.
-
-
Exercise: Regular aerobic and resistance training improves vascular tone and BP control.
-
Weight loss: Even 5–10% reduction lowers AT1R signaling burden.
-
Stress management: Meditation and yoga reduce sympathetic activation of RAAS.
2. Nutraceuticals
-
Omega 1300 — Omega 1300: Improves vascular health and reduces inflammation.
-
CoQ10 Omega — CoQ10 Omega: Enhances endothelial function.
-
Curcumin Complex — Curcumin Complex: Lowers NF-κB–mediated inflammation.
-
Magnesium: Supports vasodilation and blood pressure control.
-
Vitamin D and K2: Modulate RAAS activity and vascular calcification.
-
Resveratrol: Improves nitric oxide bioavailability and endothelial function.
3. Peptides
-
MOTS-c: Improves insulin sensitivity and vascular function.
-
BPC-157: Repairs vascular lining and reduces oxidative stress.
-
Angiotensin-(1-7) analogs: Counterbalance AT1R signaling through the Mas receptor, improving vasodilation and reducing fibrosis.
4. Medications
-
First-line:
-
ARBs (losartan, valsartan, etc.): Directly block AT1R. Particularly effective in A1166C carriers.
-
ACE inhibitors: Reduce angiotensin II levels.
-
-
Additional therapies:
-
Thiazide diuretics for sodium-sensitive hypertension.
-
Calcium channel blockers for added vasodilation.
-
Mineralocorticoid receptor antagonists (spironolactone, eplerenone) for resistant hypertension.
-
Case Example
Patient: 50-year-old male with AGTR1 A1166C AC genotype, BP 152/94 mmHg, family history of CAD. Sodium intake high.
Plan:
-
Lifestyle: DASH diet with sodium <2g/day, potassium-rich foods, aerobic exercise.
-
Supplements: Omega 1300, CoQ10 Omega, Curcumin Complex, magnesium.
-
Peptide: MOTS-c for metabolic health, BPC-157 for endothelial repair.
-
Medications: ARB initiated; thiazide diuretic added for sodium sensitivity.
-
4-month follow-up: BP 124/78, improved energy, hs-CRP reduced, carotid IMT stabilized.
The Bottom Line
The AGTR1 gene, especially the A1166C variant, strongly influences hypertension and cardiovascular disease risk through RAAS overactivation.
With CardiaX testing, clinicians can identify high-risk individuals and use precision-based interventions—lifestyle, nutraceuticals, peptides, and targeted medications—to protect cardiovascular health.
References
-
Benjafield AV, et al. AGTR1 polymorphisms and cardiovascular disease. Hypertension.
-
Tiret L, et al. A1166C polymorphism of the angiotensin II type 1 receptor gene and hypertension. Circulation.
-
Brøndum-Jacobsen P, et al. Interaction between AGTR1 variants and diet on hypertension. J Hum Hypertens.
-
Touyz RM, et al. Angiotensin II, vascular remodeling, and cardiovascular disease. Hypertension.