EKG Testing in Outpatient Care: Why a Baseline Matters for Long-Term Heart Health
Introduction
Heart disease remains the leading cause of death worldwide, but early detection can dramatically reduce risk and improve outcomes. In outpatient clinics, one of the most effective and widely available diagnostic tools is the electrocardiogram (EKG or ECG).
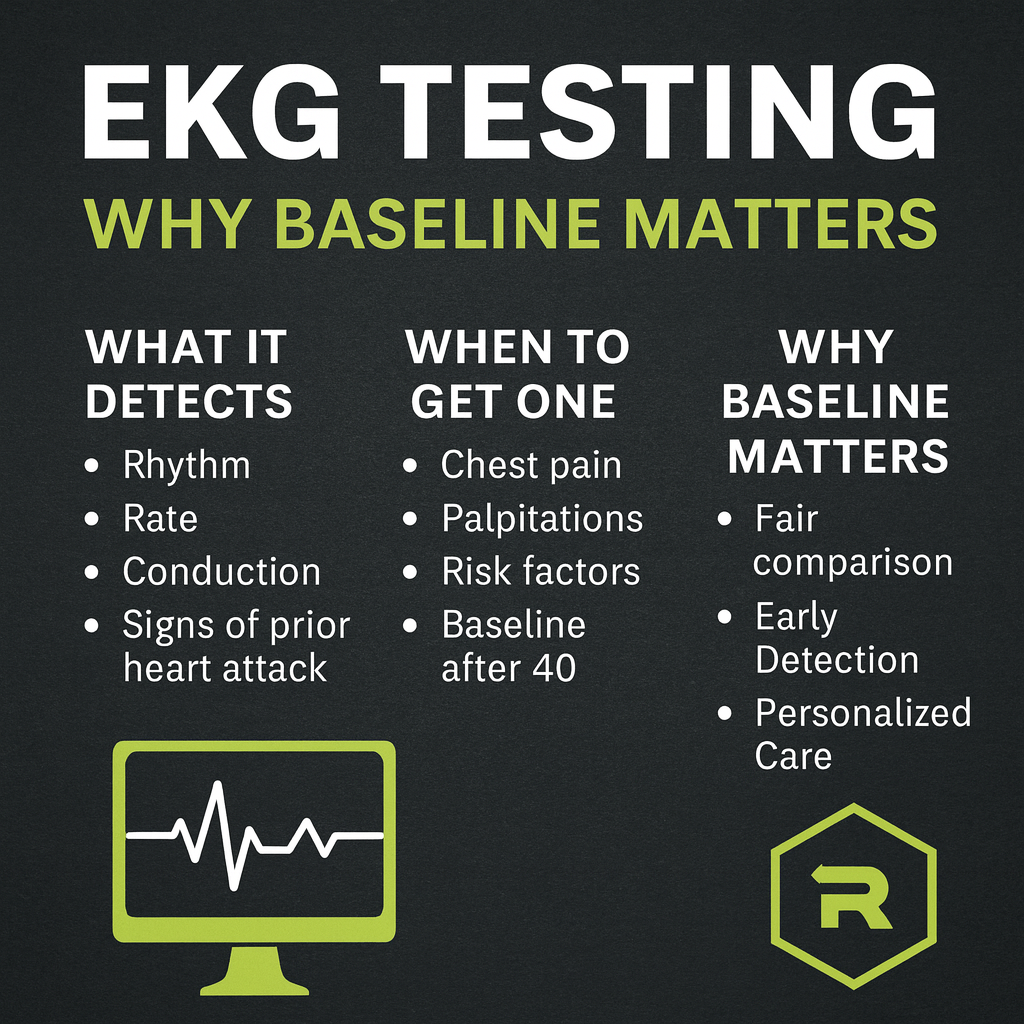
An EKG provides a snapshot of the heart’s electrical activity and can reveal arrhythmias, prior heart attacks, conduction abnormalities, and early warning signs of cardiovascular disease. Yet many patients don’t realize the importance of establishing a baseline EKG while healthy, even before any symptoms arise.
This article explores the purpose of EKG testing in outpatient clinics, why baseline EKGs are essential, and how they contribute to both prevention and long-term cardiovascular care.
What Is an EKG?
An electrocardiogram (EKG/ECG) is a non-invasive test that records the heart’s electrical activity using electrodes placed on the skin. It takes only a few minutes and produces a tracing that reflects each heartbeat’s rhythm and conduction.
-
Electro – electricity (the electrical signals generated by the heart).
-
Cardio – heart.
-
Gram – recording or tracing.
The EKG waveform provides information about:
-
Heart rhythm (regular vs. irregular)
-
Heart rate (too fast, too slow, or normal)
-
Conduction system health (how well impulses move through the heart’s electrical pathways)
-
Structural changes (such as enlargement of the heart chambers)
-
Evidence of prior injury (scarring from a previous heart attack)
Why EKGs Are Used in Outpatient Clinics
In an outpatient setting, EKGs are invaluable for both screening and diagnosis. Some of the most common reasons providers order an EKG include:
1. Evaluating Chest Pain
When a patient presents with chest discomfort, tightness, or pressure, an EKG is often the first test ordered. It can detect signs of ischemia (reduced blood flow) or a prior myocardial infarction (heart attack).
2. Assessing Palpitations or Irregular Heartbeats
Patients who feel fluttering, skipped beats, or rapid pounding may be experiencing an arrhythmia. An EKG can reveal atrial fibrillation, atrial flutter, supraventricular tachycardia, or ventricular arrhythmias.
3. Monitoring High Blood Pressure
Long-standing hypertension can cause changes in the heart’s electrical activity and structure. An EKG may reveal left ventricular hypertrophy (LVH), a thickening of the heart’s main pumping chamber.
4. Medication Monitoring
Certain medications—especially those for psychiatric conditions, infections, or cancer—can prolong the QT interval or otherwise impact the heart’s conduction system. An EKG ensures safe prescribing and monitoring.
5. Pre-Surgical Evaluation
Before surgery, a baseline EKG can assess cardiac risk and help anesthesiologists plan accordingly.
6. Annual or Preventive Screening
In preventive or executive health settings, an annual EKG may be included to catch silent abnormalities before symptoms develop.
The Importance of a Baseline EKG
Many patients only get their first EKG after symptoms appear, which limits the ability to detect subtle changes over time. By contrast, having a baseline EKG—taken when the patient is healthy—offers several advantages:
1. Detecting Silent Abnormalities
Some conditions, such as atrial fibrillation or bundle branch blocks, may not produce noticeable symptoms initially. A baseline EKG can uncover these hidden risks early.
2. Providing a Point of Comparison
If a patient later develops chest pain or palpitations, the baseline EKG allows providers to determine whether new changes are acute or chronic. For example, ST-segment changes might indicate a new heart attack—or just a stable pattern seen previously.
3. Improving Accuracy of Diagnosis
Without a baseline, interpreting EKGs can be challenging because what looks abnormal in one patient may actually be their normal pattern. A personal baseline reduces false alarms and ensures accurate diagnosis.
4. Monitoring High-Risk Patients
For patients with risk factors like hypertension, diabetes, obesity, or a family history of heart disease, a baseline EKG provides a longitudinal tool for monitoring changes over time.
5. Supporting Preventive Care
Even in healthy individuals, a baseline EKG helps establish a preventive cardiovascular profile, aligning with the principles of integrative and functional medicine.
What Conditions Can a Baseline EKG Reveal?
While a baseline EKG is not a guarantee against future events, it can highlight underlying conditions that may otherwise go unnoticed:
-
Conduction abnormalities (e.g., first-degree AV block, bundle branch block)
-
Pre-excitation syndromes (e.g., Wolff-Parkinson-White syndrome)
-
Long QT or short QT syndromes
-
Atrial fibrillation or flutter
-
Silent ischemia (reduced blood flow without obvious symptoms)
-
Chamber enlargement from hypertension or valvular disease
Who Should Get a Baseline EKG?
While not everyone requires routine EKGs, several groups particularly benefit:
-
Adults over 40 – especially if they have cardiovascular risk factors.
-
Patients with family history of sudden cardiac death or premature coronary disease.
-
Those starting new medications known to affect cardiac conduction.
-
Athletes – where hidden structural or electrical issues can increase sudden cardiac arrest risk.
-
Patients with chronic illnesses such as diabetes, kidney disease, or autoimmune conditions.
-
Individuals with unexplained symptoms like fainting, palpitations, dizziness, or exercise intolerance.
EKG vs. Other Heart Tests
An EKG is a first-line tool, but it’s often part of a broader cardiac evaluation. Understanding how it compares to other tests helps patients see why a baseline EKG is so useful.
-
EKG – Captures electrical activity at a single point in time.
-
Holter monitor – Records heart rhythm continuously for 24–48 hours.
-
Event monitor – Captures rhythm over weeks to months when symptoms occur.
-
Echocardiogram – Ultrasound that evaluates structure and pumping function.
-
Stress test – Measures how the heart responds to exercise or medication.
-
Coronary calcium score or CT angiogram – Looks at structural changes and plaque buildup.
The EKG’s advantage is its speed, affordability, and accessibility, making it the logical starting point in outpatient care.
Functional and Integrative Medicine Perspective
From a functional medicine lens, the baseline EKG is not just a diagnostic snapshot but a preventive biomarker. When combined with labs, imaging, and lifestyle assessments, it provides a more comprehensive view of cardiovascular health.
Synergy with Other Tests
-
Longevity panels (lipids, advanced cholesterol, inflammatory markers).
-
PULS test (vascular inflammation biomarkers such as IL-16, MCP-3, Fas, FasL, HGF).
-
DEXA scans for body composition and visceral fat.
-
Stress testing for metabolic flexibility.
Role of Lifestyle & Peptides
-
EKG may reveal early stress on the cardiovascular system. From there, targeted interventions like diet, exercise, and supplements can help.
-
Certain peptides under physician supervision (e.g., MOTS-c for metabolic health, BPC-157 for repair, CJC-1295/Ipamorelin for recovery) may support broader cardiovascular wellness.
How Often Should an EKG Be Repeated?
-
Baseline EKG – once in healthy adults over 40 or sooner if risk factors are present.
-
Repeat testing – every 1–2 years in high-risk patients, or sooner if new symptoms develop.
-
Pre-surgical or medication-related – as recommended by the physician.
Limitations of EKGs
While powerful, EKGs are not perfect:
-
A normal EKG does not always rule out disease (e.g., coronary blockages without electrical changes).
-
They provide a snapshot, not a continuous picture (unless combined with Holter monitoring).
-
Interpretation requires clinical context—isolated abnormalities may not be clinically significant.
Still, as part of a comprehensive cardiovascular strategy, EKGs are indispensable.
Conclusion
EKG testing is one of the simplest, most accessible, and most valuable tools in outpatient clinical care. Establishing a baseline EKG provides a foundation for comparison, helping clinicians detect changes early, prevent misdiagnosis, and personalize treatment.
Whether for prevention, monitoring, or diagnosis, the EKG remains a cornerstone of modern cardiovascular care. If you’re over 40, have risk factors, or are starting new medications, talk with your provider about getting a baseline EKG—it may prove invaluable for protecting your long-term heart health.
References
-
Hancock EW, Deal BJ, Mirvis DM, et al. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram. Circulation. 2009;119:e251–e261.
-
Rautaharju PM, Surawicz B, Gettes LS, et al. AHA/ACCF/HRS Statement: Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part IV: The ST Segment, T and U Waves, and the QT Interval. J Am Coll Cardiol. 2009;53(11):982–991.
-
American Heart Association. Electrocardiogram (EKG or ECG). Heart.org.
-
Surawicz B, Knilans TK. Chou’s Electrocardiography in Clinical Practice. 6th ed. Saunders; 2008.
-
Wagner GS, Strauss DG. Marriott’s Practical Electrocardiography. 12th ed. Wolters Kluwer; 2014.