Eotaxin and Cardiovascular Disease Risk: Understanding the Link
Cardiovascular disease (CVD) continues to be the number one cause of death worldwide. While cholesterol, blood pressure, and lifestyle choices remain important markers, they do not fully explain who develops heart attacks and strokes. Many people with “normal” labs still experience sudden cardiovascular events, which highlights the role of vascular inflammation.
The SmartVascularDx PULS test provides deeper insight by measuring seven protein biomarkers of vascular injury and inflammation, including Eotaxin. Elevated levels of this chemokine are strongly linked to vascular damage, plaque instability, and higher risk of cardiovascular events.
In this article, we’ll explore:
-
What Eotaxin is and its biological role
-
Why it matters in cardiovascular health
-
Evidence linking Eotaxin to heart disease and stroke
-
Factors that increase Eotaxin
-
Strategies to reduce Eotaxin naturally and clinically
-
Why measuring Eotaxin with the PULS test can improve prevention strategies
What Is Eotaxin?
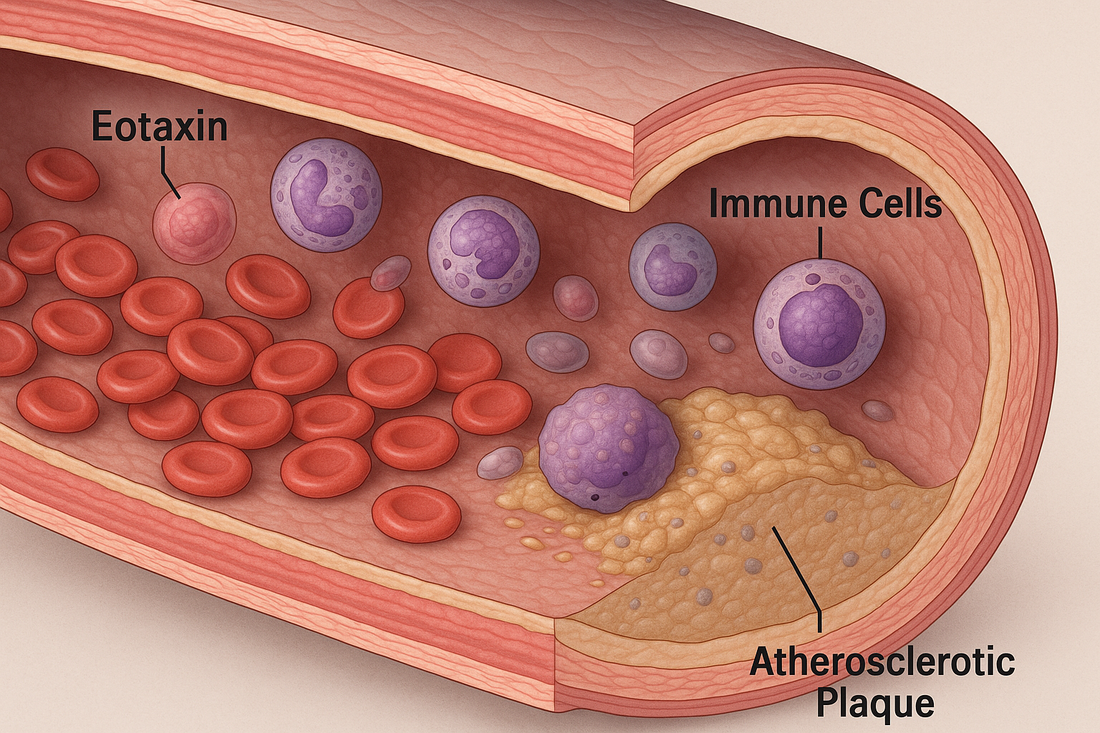
Eotaxin, also known as CCL11 (C-C motif chemokine ligand 11), is a chemokine—a signaling protein that directs immune cell movement. Its primary role is to recruit eosinophils, a type of white blood cell, to sites of inflammation or allergic response.
While eosinophils are helpful for fighting certain infections, excessive recruitment drives chronic inflammation and tissue injury.
In cardiovascular disease:
-
Eotaxin contributes to endothelial dysfunction.
-
It attracts immune cells into arterial walls.
-
It promotes fibrosis and plaque instability.
-
It has also been implicated in aging-related vascular dysfunction.
Why Eotaxin Matters in Cardiovascular Disease
Eotaxin is more than just a marker of allergy or immune activation—it plays a direct role in vascular injury and atherosclerosis.
1. Endothelial Dysfunction
Eotaxin impairs the normal function of endothelial cells (the lining of blood vessels), increasing oxidative stress and reducing nitric oxide availability. This reduces blood vessel flexibility and contributes to hypertension.
2. Atherosclerotic Plaque Formation
Eotaxin promotes the migration of eosinophils and other immune cells into vascular tissue, where they release enzymes and reactive oxygen species that damage arterial walls and foster plaque development.
3. Plaque Instability
Plaques become dangerous when they rupture. Elevated Eotaxin levels are associated with thinner fibrous caps, more inflammation, and a higher risk of rupture—leading to heart attack or stroke.
4. Biological Aging
Research shows Eotaxin levels increase with age and may impair neurogenesis and cardiovascular repair processes. High Eotaxin is often seen as a marker of accelerated biological aging.
Eotaxin and the PULS Test
The PULS test measures seven biomarkers of vascular inflammation and apoptosis: IL-16, MCP-3, CTACK, Fas, Fas Ligand, HGF, and Eotaxin.
Eotaxin’s inclusion is important because it reflects:
-
Immune-driven vascular inflammation
-
Accelerated plaque formation and remodeling
-
Higher risk of plaque rupture events
When combined with other markers, Eotaxin helps stratify patients into low, intermediate, or high risk for a major cardiovascular event within five years.
Factors That Increase Eotaxin
Eotaxin rises in response to chronic immune activation and tissue stress. Some of the most common triggers include:
1. Allergic and Atopic Conditions
Asthma, allergic rhinitis, and eczema elevate Eotaxin as part of eosinophil-driven inflammation.
2. Chronic Inflammation
-
Autoimmune diseases (rheumatoid arthritis, lupus)
-
Inflammatory bowel disease
-
Chronic infections
3. Metabolic Dysfunction
-
Obesity and visceral fat release cytokines that elevate Eotaxin.
-
Insulin resistance and diabetes accelerate vascular inflammation.
-
Dyslipidemia worsens endothelial dysfunction.
4. Cardiovascular Stress
-
Hypertension
-
Atherosclerosis
-
Heart failure
5. Environmental and Lifestyle Factors
-
Smoking
-
Air pollution exposure
-
Sedentary behavior
-
Diet high in processed foods and omega-6 oils
6. Aging
Eotaxin rises steadily with age and is considered a biomarker of immunosenescence and reduced regenerative capacity.
What Elevated Eotaxin Means for Cardiovascular Risk
High Eotaxin on the PULS test signals:
-
Active vascular inflammation
-
Higher risk of unstable plaque rupture
-
Greater likelihood of heart attack or stroke
-
Possible contribution to accelerated biological aging
How to Decrease Eotaxin and Improve Cardiovascular Health
Unlike cholesterol, which can be lowered by specific medications, Eotaxin requires a holistic approach targeting inflammation and immune dysregulation.
1. Lifestyle and Nutrition
-
Mediterranean diet – High in antioxidants, fiber, and omega-3s, it reduces vascular inflammation.
-
Reduce sugar and processed foods – Improves insulin sensitivity, lowering inflammation.
-
Exercise regularly – Both aerobic and resistance training lower systemic cytokines.
-
Quit smoking – Reduces oxidative and immune stress on arteries.
-
Improve sleep quality – Poor sleep elevates pro-inflammatory chemokines.
-
Stress reduction – Chronic stress activates inflammatory pathways linked to Eotaxin.
2. Supplements That May Lower Eotaxin
-
Omega 1300 – Reduces systemic inflammation and improves endothelial health.
-
Curcumin Complex – Shown to lower multiple inflammatory cytokines.
-
AllerFx (Quercetin) – Acts as an anti-allergic and anti-inflammatory flavonoid that downregulates chemokines like Eotaxin.
-
CoQ10 Omega – Improves mitochondrial function and reduces oxidative stress.
-
Mag Citrate – Lowers vascular stiffness and supports endothelial health.
-
ActiveMulti – Ensures micronutrient sufficiency for repair processes.
3. Peptides That May Modulate Eotaxin and Vascular Inflammation
While specific research on peptides and Eotaxin is emerging, several peptides reduce vascular inflammation and immune overactivation:
-
BPC-157 – Supports endothelial repair and reduces inflammatory signaling.
-
TB-500 – Encourages angiogenesis and vascular remodeling.
-
LL-37 – Provides antimicrobial defense, lowering chronic infection-driven inflammation.
-
KPV – Direct anti-inflammatory peptide that may suppress chemokine activity.
4. Medications That Influence Eotaxin
-
Statins – Have anti-inflammatory effects beyond lipid lowering.
-
ACE inhibitors/ARBs – Improve vascular health by reducing endothelial stress.
-
GLP-1 receptor agonists – Lower systemic inflammation in diabetes and obesity.
-
Antihistamines or leukotriene modifiers – May reduce allergy-driven Eotaxin elevations in some patients.
Eotaxin, Aging, and Longevity
Eotaxin has been studied not only in cardiovascular disease but also in aging biology. Elevated levels are associated with:
-
Reduced neurogenesis
-
Accelerated vascular aging
-
Decline in regenerative capacity
This makes Eotaxin both a CVD biomarker and a potential aging biomarker—meaning strategies to reduce it could extend both lifespan and healthspan.
Key Takeaways
-
Eotaxin (CCL11) is a chemokine that recruits eosinophils and promotes vascular inflammation.
-
Elevated levels damage the endothelium, promote plaque formation, and increase risk of rupture.
-
The PULS test measures Eotaxin to help predict 5-year cardiovascular risk.
-
Factors that raise Eotaxin include allergies, obesity, diabetes, smoking, aging, and chronic inflammation.
-
Nutrition, supplements, peptides, and medications can all help lower Eotaxin and improve vascular resilience.
Next Steps
If your PULS test shows elevated Eotaxin, it’s a sign of hidden vascular inflammation and elevated CVD risk. At Revolution Health, we use advanced cardiovascular testing, functional nutrition, and peptide therapies to reduce inflammation and stabilize plaque—helping prevent heart attacks before they happen.
References
-
Garcia-Zepeda EA, Rothenberg ME, Ownbey RT, et al. Human eotaxin is a specific chemoattractant for eosinophil cells and provides a new mechanism to explain tissue eosinophilia. Nat Med. 1996;2(4):449-456.
-
Kim CH, Broxmeyer HE. Chemokines: signal lamps for trafficking of T and B cells for development and effector function. J Leukoc Biol. 1999;65(1):6-15.
-
Yoon J, Ponikau JU, Lawrence CB, Kita H. Innate and adaptive immune responses to fungal allergens. Chem Immunol Allergy. 2006;91:48-63.
-
Luster AD. Chemokines—chemotactic cytokines that mediate inflammation. N Engl J Med. 1998;338(7):436-445.
-
Zhu J, Qiu Y, Valobra M, et al. Eotaxin (CCL11) and cardiovascular disease risk: evidence for a role in atherosclerosis progression. Atherosclerosis. 2011;219(2):573-578.
-
Humbles AA, Lu B, Friend DS, et al. The murine CCR3 receptor regulates both the role of eosinophils and mast cells in allergen-induced airway inflammation. Proc Natl Acad Sci U S A. 2002;99(3):1479-1484.
-
Huaux F. Eotaxin chemokines in eosinophil trafficking and diseases. Cytokine Growth Factor Rev. 2007;18(3-4):163-170.
-
Ueland T, Jansson AM, Nymoen SH, et al. Chemokines and cardiovascular risk prediction: a prospective cohort study. Arterioscler Thromb Vasc Biol. 2009;29(5):838-844.
-
Villeda SA, Luo J, Mosher KI, et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature. 2011;477(7362):90-94.
-
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685-1695.
-
Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368(21):2004-2013.