Food Sensitivity Testing: How to Choose the Right Panel for Your Health
Introduction: Why Food Sensitivity Testing Matters
Food has the power to heal—or to harm. For some people, everyday foods silently drive inflammation, digestive distress, skin conditions, headaches, and fatigue. The challenge is that food sensitivities are often delayed—symptoms may appear hours or even days after eating, making them very difficult to connect to a specific trigger.
That’s why advanced food sensitivity and allergy testing is so valuable. These tests measure immune responses to foods, food proteins, and food additives, providing clear insight into which items may be contributing to inflammation. With accurate testing, we can build personalized nutrition strategies, reduce systemic inflammation, and improve outcomes in autoimmune disease, gastrointestinal dysfunction, neurological conditions, and chronic fatigue.
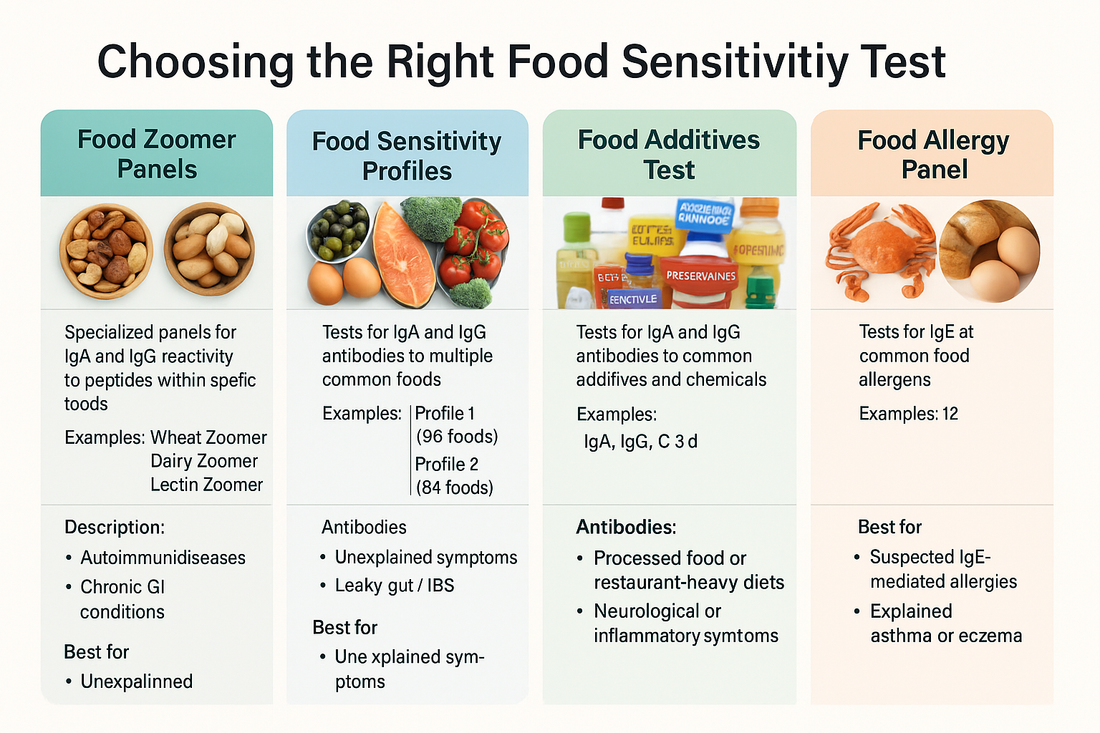
But with so many panels—Food Zoomers, Food Sensitivity Profiles, Food Additives, and Food Allergy testing—how do you know which one is right for you? This guide compares and contrasts these options so you can make an informed decision.
Understanding the Different Categories of Food Testing
1. Food Zoomer Panels
The Zoomer tests (corn, dairy, egg, grain, lectin, nut, peanut, soy, wheat) are highly specialized panels that measure IgA and IgG immune reactivity to dozens of peptides within each food group. They go deeper than standard sensitivity panels by analyzing multiple proteins within a single category, offering unmatched precision.
-
Best for: Patients with suspected autoimmune conditions, chronic GI inflammation, or persistent symptoms linked to specific food groups.
-
Examples:
-
Wheat Zoomer: comprehensive gluten/wheat protein reactivity
-
Dairy Zoomer: casein and whey sensitivity
-
Lectin Zoomer: plant lectins that drive leaky gut
-
Nut/Peanut Zoomers: tree nut vs peanut specificity
-
2. Food Sensitivity Profiles (Profiles 1 & 2, Complete)
These panels measure immune responses (IgA, IgG, and optionally IgG4/C3d) to a broad spectrum of common foods:
-
Profile 1: 96 foods
-
Profile 2: 84 foods
-
Complete: 209 foods
They give a wide survey of your immune reactivity to everyday items across categories—dairy, meat, fish, nuts, seeds, grains, fruits, and vegetables.
-
Best for: Patients with unexplained symptoms and no clear trigger foods, or those needing a broad starting point before elimination diets.
3. Food Additives Test
This test measures reactivity to 57 common food additives such as preservatives, dyes, pesticides, emulsifiers, and artificial sweeteners. Additives like MSG, aspartame, carrageenan, food dyes, and glyphosate are common in processed foods and can trigger brain fog, migraines, IBS, joint pain, and fatigue.
-
Best for: Patients who eat a lot of packaged or restaurant foods, or who have neurological or inflammatory symptoms that don’t resolve even after eliminating whole foods.
4. Food Allergy Panel
Unlike sensitivities, food allergies are IgE-mediated reactions. They can be immediate and sometimes life-threatening. This test screens for 12 of the most common food allergens, including milk, eggs, peanuts, shellfish, soy, and wheat.
-
Best for: Patients with suspected or known allergies, history of anaphylaxis, or unexplained asthma, eczema, or severe reactions.
Comparing the Antibody Types: Why They Matter
-
IgA: First line of defense at mucosal surfaces. Elevated IgA responses indicate gut-related immune activation.
-
IgG: The most abundant antibody; identifies delayed immune responses that contribute to systemic inflammation.
-
IgG4: Associated with tolerance and chronic exposure; helps determine whether a food may be less clinically relevant.
-
C3d: Indicates complement system activation, suggesting that immune responses are contributing to inflammation and tissue damage.
-
IgE: Classical allergy antibody, associated with immediate and sometimes life-threatening reactions.
Understanding which antibodies are measured helps providers interpret the clinical relevance of each test and avoid unnecessary food restrictions.
Who Should Consider Each Test?
Food Zoomer Tests
-
Autoimmune disease (celiac, Hashimoto’s, rheumatoid arthritis)
-
Chronic GI conditions (IBS, IBD, bloating, diarrhea, constipation)
-
Skin conditions (eczema, psoriasis, acne)
-
Patients who already suspect a food group (gluten, dairy, soy, etc.)
Food Sensitivity Profiles
-
Patients with broad, unexplained symptoms: brain fog, joint pain, headaches, fatigue, mood swings
-
Those with leaky gut, chronic inflammation, or IBS
-
A first-line screen for patients unsure where to start
Food Additives Test
-
Patients who consume processed foods or restaurant meals frequently
-
Those with migraines, ADHD, brain fog, skin flares, or asthma-like symptoms
-
Patients with persistent symptoms despite eliminating common whole-food triggers
Food Allergy Panel
-
Patients with suspected IgE-mediated food allergies
-
Children with eczema, asthma, or recurrent ear infections
-
Adults with unexplained rashes, swelling, or anaphylaxis
-
Those with a strong family history of food allergies
How Food Sensitivity Testing Improves Clinical Outcomes
Food testing is not just about avoiding foods—it’s about removing immune triggers to reduce inflammation and restore function. Clinical applications include:
-
Gastrointestinal healing: Removing reactive foods calms inflammation, reduces bloating/diarrhea/constipation, and restores the gut barrier.
-
Autoimmune disease management: Lowering immune load decreases symptom flares in conditions like celiac, rheumatoid arthritis, lupus, and MS.
-
Neurological support: Brain fog, migraines, ADHD, and mood symptoms often improve when sensitivities are addressed.
-
Skin conditions: Eczema, acne, hives, and psoriasis commonly improve with tailored elimination.
-
Energy and metabolism: Reduced inflammation supports mitochondrial function and decreases fatigue.
How to Choose the Right Test
Step 1: Identify Your Main Symptoms
-
Digestive distress → Start with Gut Zoomer + Food Sensitivity Profile or Zoomers.
-
Neurological symptoms (brain fog, migraines) → Consider Food Additives Test.
-
Skin rashes, swelling, or anaphylaxis → Food Allergy Panel.
-
Autoimmune disease → Wheat Zoomer, Dairy Zoomer, or Lectin Zoomer.
Step 2: Consider Diet & Lifestyle
-
If you eat a wide range of whole foods: Sensitivity Profile or Complete panel.
-
If your diet is processed or restaurant-heavy: Additives panel.
-
If you already suspect a food group: Zoomer panel for that food.
Step 3: Work with a Provider
-
Results must be interpreted in the context of symptoms, history, and gut health.
-
A provider can build a structured elimination and reintroduction plan instead of unnecessary long-term restriction.
Conclusion: Testing, Not Guessing
Food sensitivities, additives, and allergies play a powerful role in chronic health conditions. Because symptoms are delayed, vague, or mimic other diseases, identifying food triggers without testing is nearly impossible.
By using the right test—whether a Zoomer, Food Sensitivity Profile, Food Additives, or Food Allergy panel—we can identify the foods and additives driving inflammation, remove them strategically, and support gut healing. This approach not only relieves symptoms but also improves long-term outcomes in autoimmunity, GI disorders, skin disease, and neurological health.
The right test is the first step toward building a personalized nutrition plan that restores energy, reduces inflammation, and helps you feel like yourself again.
References
-
Vibrant Wellness. Food Sensitivity Tests: Key Clinical Messages
-
Vibrant Wellness. Food Additives Test: Key Clinical Messages
-
Vibrant Wellness. Food Additives Patient One-Pager
-
Vibrant Wellness. Food Sensitivity Profile 1
-
Vibrant Wellness. Food Sensitivity Profile 2
-
Vibrant Wellness. Food Allergy Panel: Key Clinical Messages