Hepatocyte Growth Factor (HGF) and Cardiovascular Disease Risk: What You Need to Know
Cardiovascular disease (CVD) is the leading cause of death worldwide, and despite advances in cholesterol management, blood pressure treatment, and lifestyle interventions, many individuals still suffer unexpected heart attacks or strokes. That’s because traditional risk factors don’t tell the full story—they miss hidden vascular inflammation and plaque instability.
The SmartVascularDx PULS test addresses this gap by measuring seven key protein biomarkers of vascular injury and inflammation. Among them is Hepatocyte Growth Factor (HGF), a marker of endothelial damage and tissue remodeling that plays a pivotal role in cardiovascular risk assessment.
In this article, we’ll explore:
-
What HGF is and its physiological role
-
Why it matters in cardiovascular health
-
Evidence linking elevated HGF to plaque instability and CVD risk
-
Factors that increase HGF
-
Strategies to reduce HGF naturally and clinically
-
How monitoring HGF can improve prevention and treatment strategies
What Is Hepatocyte Growth Factor (HGF)?
Hepatocyte Growth Factor (HGF) is a pleiotropic cytokine primarily secreted by mesenchymal cells. Originally discovered as a liver regenerative factor, HGF is now recognized as a broad tissue repair and angiogenesis regulator.
HGF binds to its receptor, c-Met, triggering a cascade of signals that promote:
-
Cell growth and survival
-
Angiogenesis (new blood vessel formation)
-
Tissue regeneration
-
Wound healing
In the cardiovascular system, HGF is protective in acute injury, helping restore blood supply and repair damaged tissue. However, chronically elevated HGF indicates ongoing vascular injury and remodeling—a hallmark of unstable atherosclerotic plaque.
Why HGF Matters in Cardiovascular Disease
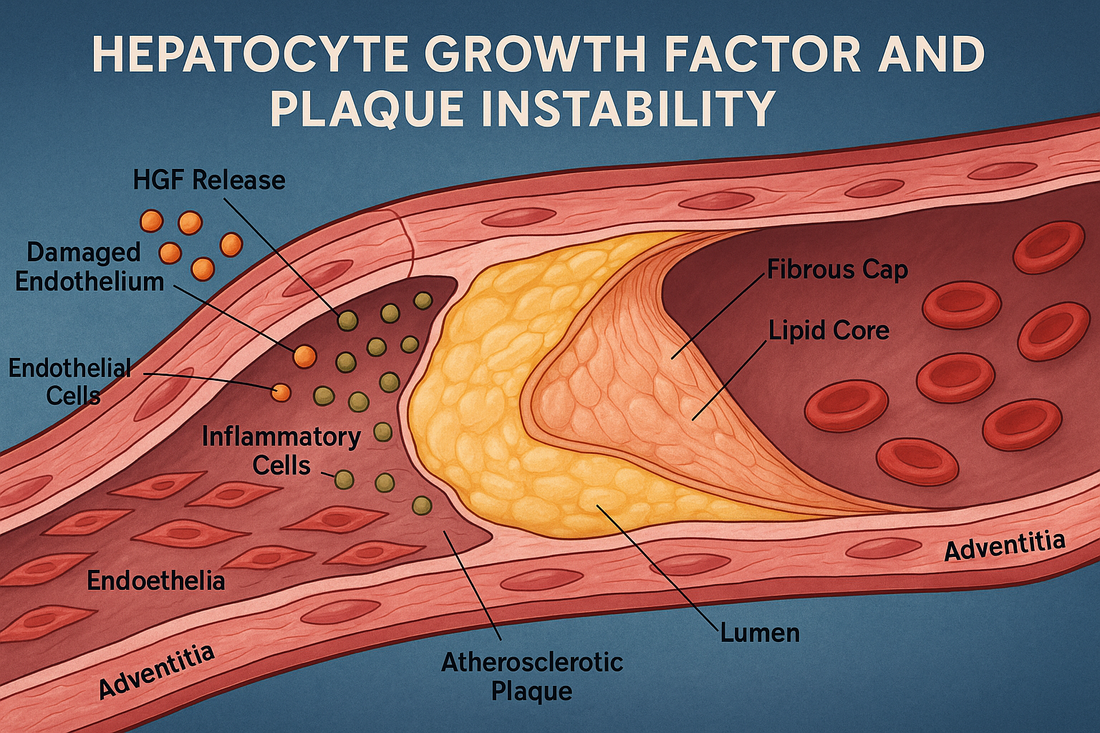
1. Endothelial Dysfunction
The endothelium (inner lining of blood vessels) releases HGF in response to injury. High HGF reflects ongoing vascular stress, which accelerates atherosclerosis.
2. Plaque Instability
Unstable atherosclerotic plaques have thinner fibrous caps and are prone to rupture. Elevated HGF correlates with plaque remodeling and instability—making it a strong predictor of acute coronary syndromes.
3. Inflammation and Fibrosis
Chronic inflammation drives both HGF release and vascular fibrosis. Persistent HGF signaling indicates an environment of repair attempts that cannot keep up with injury.
4. Prognostic Value
High HGF levels are associated with:
-
Increased risk of myocardial infarction
-
Higher incidence of stroke
-
Faster progression of atherosclerosis
-
All-cause mortality in patients with CVD
HGF and the PULS Test
The PULS test measures seven biomarkers: IL-16, MCP-3, Eotaxin, CTACK, Fas, Fas Ligand, and HGF. Together, they create a composite score predicting a 5-year risk of heart attack.
HGF’s inclusion is critical because it reflects:
-
Endothelial damage
-
Vascular remodeling stress
-
Ongoing attempts at healing after injury
In patients with otherwise “normal” cholesterol and blood pressure, elevated HGF may reveal hidden vulnerability to plaque rupture, giving clinicians a chance to intervene earlier.
Factors That Increase HGF
HGF is upregulated in conditions where the body perceives chronic tissue stress or injury. Common drivers include:
1. Cardiovascular Stressors
-
Hypertension → damages the endothelium, increasing HGF.
-
Atherosclerosis → plaques cause constant vascular remodeling.
-
Heart failure → myocardial stress stimulates HGF release.
2. Metabolic Dysfunction
-
Obesity and visceral fat secrete cytokines that elevate HGF.
-
Insulin resistance & diabetes accelerate endothelial injury.
-
Dyslipidemia (especially oxidized LDL) upregulates HGF signaling.
3. Chronic Inflammation
-
Autoimmune disease
-
Chronic infections
-
Persistent low-grade inflammation from poor diet or toxins
4. Lifestyle Factors
-
Smoking – Direct endothelial damage increases HGF expression.
-
Excess alcohol – Damages vascular and liver tissues.
-
Sedentary lifestyle – Increases systemic inflammation, reducing vascular resilience.
5. Aging
Aging vessels show chronic HGF activation as a compensatory but insufficient repair mechanism.
What Elevated HGF Means for Your Heart
When HGF is elevated on the PULS test, it suggests endothelial injury and unstable plaque dynamics. This makes patients more vulnerable to:
-
Plaque rupture → heart attack or stroke
-
Faster progression of coronary artery disease
-
Microvascular dysfunction (impaired small vessel health)
-
Reduced vascular resilience with aging
How to Decrease HGF and Reduce CVD Risk
The goal is not to eliminate HGF—it plays a protective role in acute injury. Instead, the aim is to reduce chronic overactivation by addressing underlying causes of vascular inflammation and injury.
1. Nutrition & Lifestyle
-
Adopt an anti-inflammatory diet – Mediterranean-style eating lowers vascular stress.
-
Reduce sugar & refined carbs – Improves insulin sensitivity and endothelial health.
-
Quit smoking – Immediate reduction in endothelial injury.
-
Exercise regularly – Both aerobic and resistance training reduce systemic inflammation.
-
Stress reduction – Meditation, HRV training, and restorative sleep lower inflammatory signals.
2. Supplements That Support Lower HGF
-
Omega 1300 – Reduces vascular inflammation and improves endothelial function.
-
Curcumin Complex – Potent anti-inflammatory that downregulates cytokines driving HGF.
-
AllerFx (Quercetin) – Improves vascular signaling and reduces endothelial apoptosis.
-
CoQ10 Omega – Protects mitochondria in vascular cells.
-
Mag Citrate – Low magnesium increases endothelial dysfunction.
-
ActiveMulti – Ensures micronutrient sufficiency for repair without excess inflammatory activation.
3. Peptide Therapies That May Help Normalize HGF
Several peptides offered at Revolution Health support vascular health and may indirectly modulate HGF levels:
-
BPC-157 – Promotes endothelial repair and reduces chronic vascular inflammation.
-
TB-500 – Supports angiogenesis and vascular remodeling balance.
-
LL-37 – Reduces chronic infection load that can drive HGF.
-
KPV – Anti-inflammatory peptide reducing cytokine pathways tied to endothelial stress.
4. Medications That Influence HGF
-
Statins – Anti-inflammatory effects beyond cholesterol lowering.
-
ACE inhibitors/ARBs – Improve endothelial function and reduce vascular stress.
-
GLP-1 receptor agonists (e.g., semaglutide, retatrutide in trial) – Reduce inflammation and improve endothelial health.
-
SGLT2 inhibitors – Improve vascular and metabolic stress.
HGF, Longevity, and Cardiovascular Prevention
HGF represents the body’s attempt at vascular repair—but when elevated chronically, it signals unresolved injury and high risk of plaque rupture. By lowering chronic vascular inflammation through precision medicine strategies, HGF can normalize, reflecting improved endothelial resilience.
Key Takeaways
-
HGF (Hepatocyte Growth Factor) is a biomarker of endothelial injury and vascular remodeling.
-
Chronically high HGF is linked to unstable plaque and higher CVD risk.
-
The PULS test includes HGF as a critical marker for predicting 5-year heart attack risk.
-
Elevated HGF reflects oxidative stress, metabolic dysfunction, inflammation, smoking, and aging.
-
Lifestyle changes, targeted supplements, peptides, and medications can lower HGF and improve vascular health.
Next Steps
If your PULS test shows elevated HGF, don’t ignore it. At Revolution Health, we use advanced cardiovascular testing, functional medicine nutrition, and peptide therapies to lower vascular inflammation and prevent heart attacks before they happen.
Your cardiovascular risk is not fixed—it can be reversed with the right strategy.
References
-
Nakamura T, Nawa K, Ichihara A. Partial purification and characterization of hepatocyte growth factor from serum of hepatectomized rats. Biochem Biophys Res Commun. 1984;122(3):1450-1459.
-
Nakamura T, Mizuno S. The discovery of hepatocyte growth factor (HGF) and its significance for cell biology, life sciences and clinical medicine. Proc Jpn Acad Ser B Phys Biol Sci. 2010;86(6):588-610.
-
Matsumoto K, Nakamura T. Hepatocyte growth factor and the Met system as a mediator of tumor–stromal interactions. Int J Cancer. 2006;119(3):477-483.
-
Nakamura Y, Morishita R, Higaki J, et al. Hepatocyte growth factor as a potential index of severity of coronary artery disease. Circulation. 2000;102(7):769-774.
-
Pulkki K, Pelliniemi TT, Laine J, et al. Elevated circulating hepatocyte growth factor is associated with unstable angina and myocardial infarction. Circulation. 1997;96(3):821-826.
-
Funatsu H, Yamashita H, Ikeda T, Mimura T. Vitreous levels of hepatocyte growth factor and vascular endothelial growth factor are increased in patients with diabetic retinopathy. Diabetes Care. 2003;26(3):1007-1011.
-
Patel N, Basheer HA, Daly C, et al. Hepatocyte growth factor in cardiovascular disease: a potential therapeutic target. Curr Vasc Pharmacol. 2014;12(5):786-797.
-
Ueda K, Ueda Y, Matsumoto K, et al. Increased circulating hepatocyte growth factor in patients with acute myocardial infarction. Am Heart J. 1996;132(5):1020-1024.
-
Gallo S, Sala V, Gatti S, Crepaldi T. HGF/Met axis in heart function and cardioprotection. Biomedicines. 2014;2(4):247-262.
-
Gallego MJ, Rojas A. Cardioprotective role of hepatocyte growth factor in cardiovascular disease. J Cardiovasc Dev Dis. 2020;7(2):17.
-
Nakamura Y, Morishita R, Higaki J. Increased hepatocyte growth factor predicts cardiovascular events in patients with coronary artery disease. Am J Cardiol. 2001;88(8):866-869.
-
Sugimachi M, Iwai M, Yamamoto K, et al. Circulating hepatocyte growth factor is increased in patients with hypertension. Hypertension. 1997;30(3):495-499.
-
Oh H, Takagi H, Takagi C, Suzuma K, Otani A, Ishida K, Matsumura M. Elevated HGF in patients with diabetic nephropathy. Diabetes. 2000;49(3):617-622.
-
Minami S, Kijima H, Takahashi T, et al. Circulating hepatocyte growth factor as a novel marker of vascular injury in atherosclerosis. Atherosclerosis. 1999;142(1):169-177.
-
Libby P. Inflammation and atherosclerosis. Nature. 2002;420(6917):868-874.