MCP-3 (CCL7) and Cardiovascular Disease Risk: The Inflammatory Link
Introduction
Cardiovascular disease (CVD) remains the world’s leading cause of death, fueled in part by chronic inflammation. While cholesterol, blood pressure, and glucose levels dominate clinical attention, newer research has highlighted the importance of inflammatory cytokines and chemokines in shaping cardiovascular risk.
Among these is Monocyte Chemoattractant Protein-3 (MCP-3), also called CCL7, a signaling molecule that recruits immune cells to sites of tissue injury or infection. MCP-3 belongs to the CC chemokine family and has been increasingly studied as a biomarker of vascular inflammation and plaque instability.
This article explores MCP-3’s role in cardiovascular disease, the factors that increase its levels, and the strategies that may help lower its impact on long-term heart health.
What Is MCP-3?
MCP-3 is a chemokine, a class of small proteins that guide the movement of immune cells. Specifically, MCP-3 attracts monocytes, T lymphocytes, basophils, and natural killer cells to sites of inflammation.
It binds to multiple chemokine receptors, including CCR1, CCR2, CCR3, and CCR5, giving it broad influence over the immune system. Unlike other chemokines that act more selectively, MCP-3’s ability to interact with several receptor pathways makes it a potent amplifier of immune signaling.
While MCP-3 is necessary for normal host defense, sustained elevation contributes to chronic inflammation—a hallmark of cardiovascular disease.
MCP-3 and Atherosclerosis
Atherosclerosis is now recognized as an inflammatory disease of the arteries. The process begins with endothelial dysfunction and low-grade immune activation, followed by lipid accumulation, immune cell infiltration, and eventually plaque development.
MCP-3 plays several roles in this progression:
-
Monocyte Recruitment: MCP-3 draws monocytes into the arterial wall, where they differentiate into macrophages and engulf oxidized LDL cholesterol, forming foam cells.
-
Plaque Progression: Elevated MCP-3 levels correlate with greater inflammatory cell content in plaques, which contributes to instability and rupture.
-
Vascular Remodeling: MCP-3 influences smooth muscle cell migration and proliferation, shaping vessel structure during chronic injury.
-
Systemic Inflammation Marker: Circulating MCP-3 levels are higher in individuals with advanced atherosclerosis, suggesting it reflects the burden of vascular inflammation.
MCP-3 Beyond the Heart: Broader Health Impacts
MCP-3 is not only relevant to cardiovascular health. It is also implicated in:
-
Obesity and Insulin Resistance: Adipose tissue produces MCP-3, linking excess weight to metabolic and vascular inflammation.
-
Autoimmune Diseases: Elevated MCP-3 is observed in lupus, rheumatoid arthritis, and multiple sclerosis.
-
Infections: Viral and bacterial infections can drive MCP-3 release, mobilizing immune cells.
-
Cancer Biology: MCP-3 participates in tumor microenvironments by shaping immune infiltration.
These findings highlight MCP-3 as a general inflammation signal, which may explain its predictive value in cardiovascular risk panels like the PULS test.
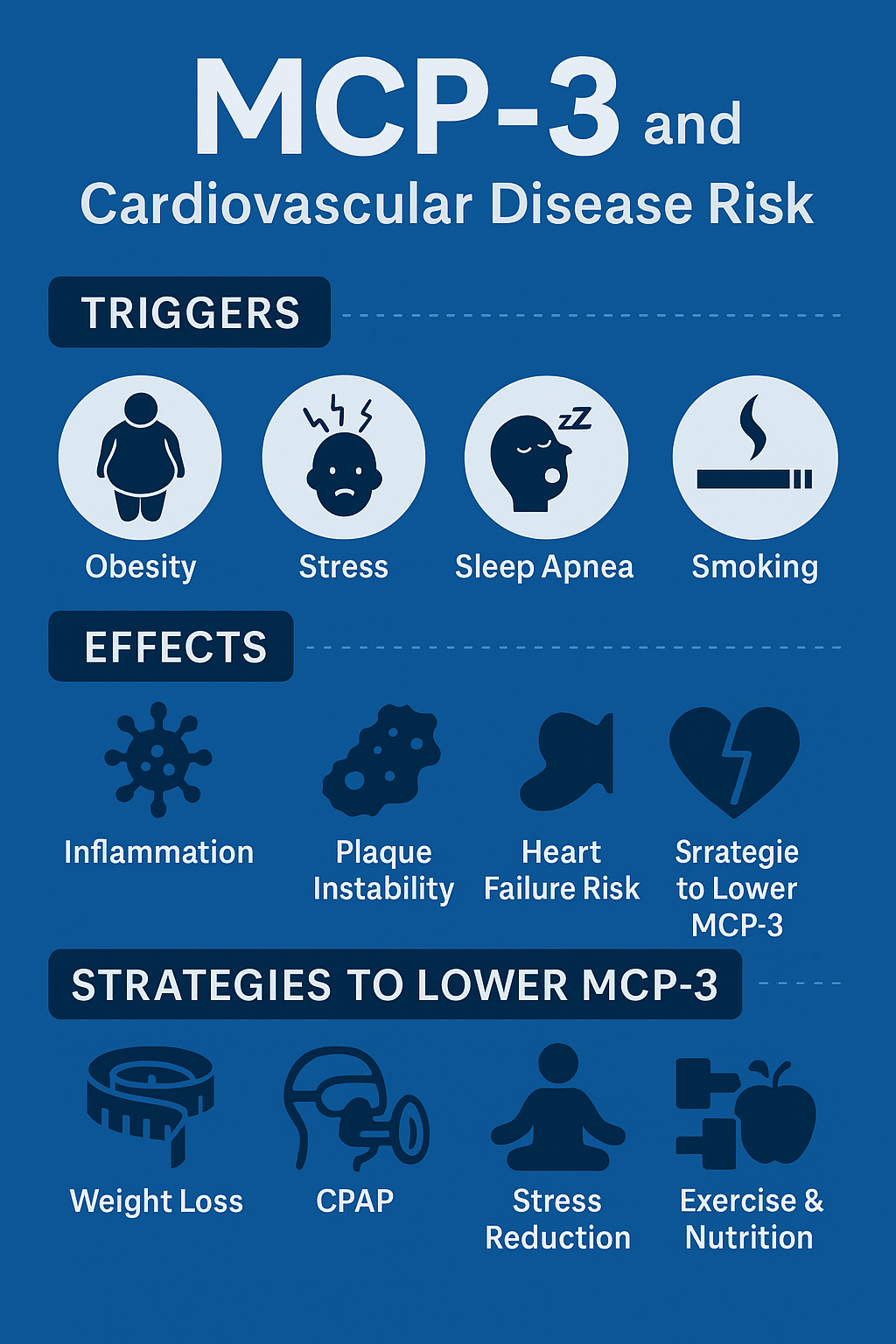
What Elevates MCP-3?
Several lifestyle, metabolic, and environmental factors can raise MCP-3 levels:
1. Obesity
Excess visceral fat is metabolically active, producing pro-inflammatory cytokines and chemokines, including MCP-3. Adipose tissue macrophages secrete MCP-3, creating a vicious cycle of inflammation and insulin resistance.
2. Diabetes and Insulin Resistance
High glucose and advanced glycation end products stimulate MCP-3 release, accelerating vascular injury. Individuals with poorly controlled diabetes often show elevated chemokine profiles.
3. Stress
Chronic stress increases sympathetic nervous system activity and cortisol dysregulation, which can trigger pro-inflammatory cytokine release. MCP-3 is part of this stress-induced inflammatory cascade.
4. Sleep Apnea
Obstructive sleep apnea causes intermittent hypoxia, oxidative stress, and systemic inflammation. These conditions elevate inflammatory markers, and MCP-3 is likely among them, though direct studies remain limited.
5. Smoking
Cigarette smoke introduces oxidative stress and endothelial injury, upregulating MCP-3 expression in the vascular wall.
6. Infections
Respiratory viruses and bacterial infections activate MCP-3 pathways, sometimes contributing to transient cardiovascular risk increases after illness.
7. Aging and “Inflammaging”
MCP-3 levels appear to rise with age as part of chronic low-grade inflammation that contributes to vascular disease progression.
MCP-3 and Cardiovascular Outcomes
Atherosclerotic Plaques
Histological studies have found MCP-3 enriched in unstable plaques, often co-localized with macrophages and foam cells. This suggests a role in driving plaque rupture, the immediate cause of heart attacks and strokes.
Heart Failure
MCP-3 is elevated in patients with heart failure, reflecting ongoing inflammatory activity. Elevated MCP-3 may worsen myocardial remodeling by promoting immune infiltration.
Post-Myocardial Infarction Remodeling
After a heart attack, MCP-3 is released as part of the repair process. While necessary acutely, sustained elevation contributes to maladaptive remodeling and heart failure risk.
Strategies to Lower MCP-3
Since MCP-3 is an inflammation marker, strategies to reduce it often target upstream drivers of inflammation.
Lifestyle Interventions
-
Weight Loss
-
Reduces adipose tissue-derived cytokines and chemokines.
-
Bariatric surgery and lifestyle modification both lower systemic inflammatory markers, likely including MCP-3.
-
Exercise
-
Regular aerobic activity reduces vascular inflammation and improves endothelial health.
-
Resistance training lowers pro-inflammatory cytokines and enhances insulin sensitivity.
-
Dietary Approaches
-
Anti-inflammatory diets (Mediterranean, plant-forward, low processed foods).
-
Key nutrients: omega-3 fatty acids, polyphenols (curcumin, quercetin), and fiber.
-
Supplements such as Omega 1300, Curcumin Complex, and AllerFx (quercetin) may help regulate cytokine production.
-
Sleep Optimization
-
Treating sleep apnea with CPAP reduces systemic inflammation.
-
Adequate restorative sleep improves immune balance and reduces cytokine load.
-
Stress Management
-
Meditation, breathwork, yoga, and therapy all reduce stress-induced cytokine release.
-
Chronic stress is a powerful driver of inflammatory pathways.
Medical and Pharmacological Approaches
-
Statins
-
Beyond cholesterol lowering, statins have anti-inflammatory effects and may lower chemokines like MCP-3.
-
ACE Inhibitors/ARBs
-
Improve endothelial function and reduce cytokine signaling.
-
Anti-Cytokine Therapies
-
Experimental approaches targeting IL-1β, IL-6, and TNF pathways show proof of concept that chemokine suppression reduces cardiovascular risk. MCP-3-specific therapies are not yet available but may emerge.
-
Metabolic Therapies
-
GLP-1 receptor agonists (like semaglutide and retatrutide) reduce weight and inflammation.
-
Peptide therapies such as MOTS-c improve mitochondrial health, which lowers oxidative stress and inflammatory signaling.
Future Directions
MCP-3 holds promise as a cardiovascular biomarker that captures risk beyond traditional lipid measurements. Incorporating MCP-3 into multi-marker panels (like the PULS test) may help identify patients at near-term risk for cardiac events, even when cholesterol appears normal.
Future research priorities include:
-
Determining how strongly MCP-3 predicts cardiovascular events compared with other cytokines.
-
Clarifying whether lowering MCP-3 directly improves outcomes.
-
Developing targeted therapies to modulate MCP-3 activity safely.
Conclusion
MCP-3 (CCL7) is a powerful chemokine that orchestrates immune cell recruitment and amplifies inflammation. In cardiovascular disease, it contributes to atherosclerosis progression, plaque instability, and post-MI remodeling.
Factors that elevate MCP-3 include obesity, diabetes, stress, sleep apnea, smoking, infections, and aging. Fortunately, lifestyle strategies—weight management, exercise, anti-inflammatory nutrition, stress reduction, and sleep optimization—along with medical therapies can help reduce its levels and protect cardiovascular health.
As research continues, MCP-3 may emerge as both a diagnostic tool and a therapeutic target, offering new ways to reduce the global burden of heart disease.
References
-
Charo IF, Ransohoff RM. The many roles of chemokines and chemokine receptors in inflammation. N Engl J Med. 2006;354(6):610-621.
-
Dewald O, Ren G, Duerr GD, et al. Of mice and dogs: species-specific differences in the inflammatory response following myocardial infarction. Am J Pathol. 2004;164(2):665-677.
-
Gosling J, Slaymaker S, Gu L, et al. MCP-1 deficiency reduces susceptibility to atherosclerosis in mice that overexpress human apolipoprotein B. J Clin Invest. 1999;103(6):773-778.
-
Jiang Y, Valente AJ, Zhou Q, et al. Multiple roles of the chemokine monocyte chemoattractant protein-3 (MCP-3) in cardiovascular disease. Cytokine. 2020;136:155260.
-
Zernecke A, Weber C. Chemokines in atherosclerosis: proceedings resumed. Arterioscler Thromb Vasc Biol. 2014;34(4):742-750.
-
Ylä-Herttuala S, Lipton BA, Rosenfeld ME, et al. Expression of monocyte chemoattractant protein-1 in macrophage-rich areas of human and rabbit atherosclerotic lesions. Proc Natl Acad Sci USA. 1991;88(12):5252-5256.
-
Apostolakis S, Vogiatzi K, Krambovitis E, Spandidos DA. Chemokines in vascular pathology (review). Int J Mol Med. 2006;17(5):691-701.
-
Kanda H, Tateya S, Tamori Y, et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Invest. 2006;116(6):1494-1505.
-
Harada A, Sekido N, Akahoshi T, Wada T, Mukaida N, Matsushima K. Essential involvement of interleukin-8 (IL-8) in acute inflammation. J Leukoc Biol. 1994;56(5):559-564.
-
Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12(3):204-212.
-
Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119-1131.
-
Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32(9):2045-2051.
-
Kim JB, Zaidi SH, McCarthy BP, et al. MCP-3 is a novel biomarker of plaque vulnerability associated with impaired vascular function. Atherosclerosis. 2018;269:100-107.
-
Braunersreuther V, Zernecke A, Arnaud C, et al. CCL5/RANTES inhibition reduces atherosclerotic plaque development in mice. Arterioscler Thromb Vasc Biol. 2007;27(4):857-865.
-
Singh MV, Chapleau MW, Harwani SC, Abboud FM. The immune system and hypertension. Immunol Res. 2014;59(1-3):243-253.