MTHFR Gene Variants: A Central Player in Cardiovascular Health
Introduction
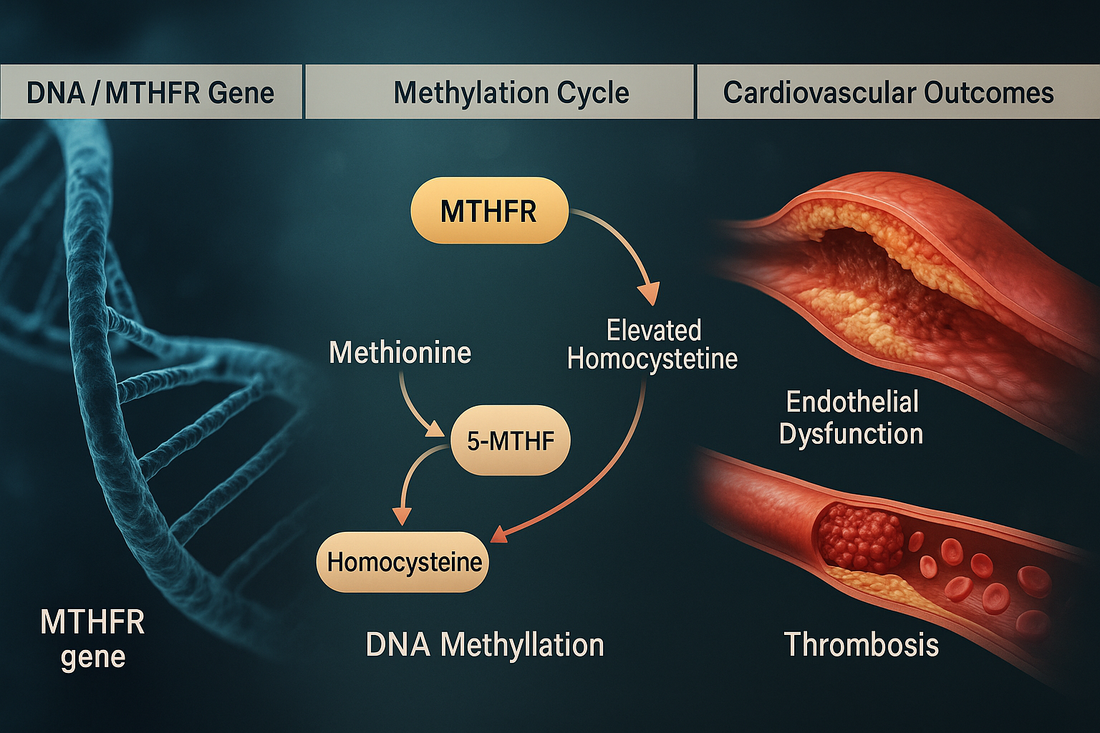
The methylenetetrahydrofolate reductase (MTHFR) gene, located on chromosome 1p36, encodes an enzyme critical for folate metabolism and homocysteine clearance. Through its role in the methylation cycle, MTHFR maintains vascular integrity, DNA synthesis, and neurotransmitter balance.
Two common polymorphisms—C677T (rs1801133) and A1298C (rs1801131)—reduce enzyme activity, leading to elevated homocysteine and impaired methylation. Both have been linked to cardiovascular disease (CVD), hypertension, stroke, and thrombosis risk.
Your CardiaX test identifies whether you carry these variants, enabling proactive interventions.
MTHFR and the Methylation Cycle
-
Normal role: MTHFR converts 5,10-methylene-tetrahydrofolate into 5-methyltetrahydrofolate (5-MTHF), the active folate required for homocysteine → methionine conversion.
-
Methionine: Used to generate S-adenosylmethionine (SAMe), the universal methyl donor for DNA, neurotransmitters, and detoxification.
-
Disruption: MTHFR variants impair this process, causing homocysteine accumulation and reduced methylation potential.
MTHFR Variants and Their Effects
C677T (rs1801133)
-
TT homozygotes: 30–35% enzyme activity.
-
CT heterozygotes: ~65% activity.
-
CC homozygotes: Normal.
-
Clinical impact:
-
Elevated homocysteine.
-
Increased risk of hypertension, atherosclerosis, venous thrombosis, and stroke.
-
A1298C (rs1801131)
-
CC homozygotes: 60–70% enzyme activity.
-
AC heterozygotes: Mild reduction.
-
AA homozygotes: Normal.
-
Clinical impact:
-
Less effect on homocysteine than C677T.
-
Impacts neurotransmitter metabolism and nitric oxide regulation.
-
Contributes to CVD risk when combined with C677T.
-
Compound Heterozygotes (C677T + A1298C)
-
Significantly reduced MTHFR function.
-
Higher cardiovascular and clotting risk.
MTHFR and Cardiovascular Disease
-
Elevated Homocysteine
-
Directly damages endothelial lining.
-
Promotes LDL oxidation and plaque formation.
-
Increases platelet aggregation and clot risk.
-
-
Methylation Deficiency
-
Impaired detoxification of estrogens, toxins, and neurotransmitters.
-
Reduced nitric oxide bioavailability → vascular stiffness.
-
DNA hypomethylation → inflammatory gene expression.
-
-
Vascular Remodeling
-
Chronic homocysteine burden leads to smooth muscle proliferation and atherosclerosis.
-
What Exacerbates Risk in MTHFR Variants?
-
Folate deficiency (low leafy greens, low supplementation).
-
Low vitamin B12 or B6 status.
-
High alcohol intake (depletes folate).
-
Smoking (oxidative stress increases homocysteine toxicity).
-
Sedentary lifestyle.
-
High refined carbohydrate intake (worsens methyl donor deficiency).
How to Mitigate MTHFR-Associated Risk
1. Lifestyle Strategies
-
Folate-rich diet: Leafy greens, legumes, asparagus, avocado.
-
Limit alcohol: Preserves folate and methylation capacity.
-
Exercise: Improves vascular flexibility and lowers homocysteine.
-
Avoid smoking: Protects vascular endothelium.
2. Nutraceuticals
-
Methyl Protect — Provides methylated B12, 5-MTHF, betaine, and B6.
-
CoQ10 Omega — CoQ10 Omega: Improves endothelial function.
-
Mag Glycinate: Supports methylation and vascular health.
-
Curcumin Complex — Curcumin Complex: Anti-inflammatory and antioxidant.
-
N-acetylcysteine (NAC): Boosts glutathione and supports detoxification.
3. Peptide Therapies
-
BPC-157: Heals vascular damage from oxidative stress.
-
MOTS-c: Enhances mitochondrial function, reduces oxidative burden.
-
KPV: Anti-inflammatory and protects endothelium.
4. Medications
-
Folate/B-vitamin therapy: Clinical-grade methylated folate and B12 supplements.
-
Beta-blockers or ACE inhibitors: For hypertension management.
-
Antiplatelet therapy: For those with prior clotting history and elevated homocysteine.
Case Example
A 42-year-old woman with MTHFR C677T homozygous (TT) presented with elevated homocysteine (18 µmol/L), hypertension, and family history of stroke.
Plan:
-
Nutraceuticals: Methyl Protect, CoQ10 Omega, NAC.
-
Lifestyle: Mediterranean diet, reduced alcohol, exercise.
-
Peptide: BPC-157 prescribed for vascular repair.
-
Medication: Started on low-dose folate + B12 combination therapy.
Outcome: Homocysteine reduced to 8 µmol/L within 6 months, blood pressure normalized, improved vascular health markers.
The Bottom Line
The MTHFR gene polymorphisms (C677T and A1298C) significantly affect cardiovascular health by disrupting methylation and increasing homocysteine.
-
C677T: Stronger effect on homocysteine and vascular risk.
-
A1298C: Milder, but impacts neurotransmitters and nitric oxide.
-
Compound heterozygotes: Highest overall cardiovascular risk.
CardiaX testing allows personalized interventions—ranging from diet to targeted supplements, peptides, and medications—to reduce risk and restore balance.
References
-
Frosst P, et al. A candidate genetic risk factor for vascular disease: a common mutation in MTHFR. Nat Genet. 1995.
-
Humphrey LL, et al. Homocysteine level and coronary heart disease: a systematic review and meta-analysis. JAMA. 2008.
-
Wald DS, et al. Homocysteine and cardiovascular disease: evidence on causality. BMJ. 2006.
-
Liew SC, Gupta ED. Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: epidemiology, metabolism and the associated diseases. Eur J Med Genet. 2015.