Prolotherapy for Shoulder Instability After Dislocation: A Non-Surgical Regenerative Solution
Understanding Shoulder Instability After Dislocation
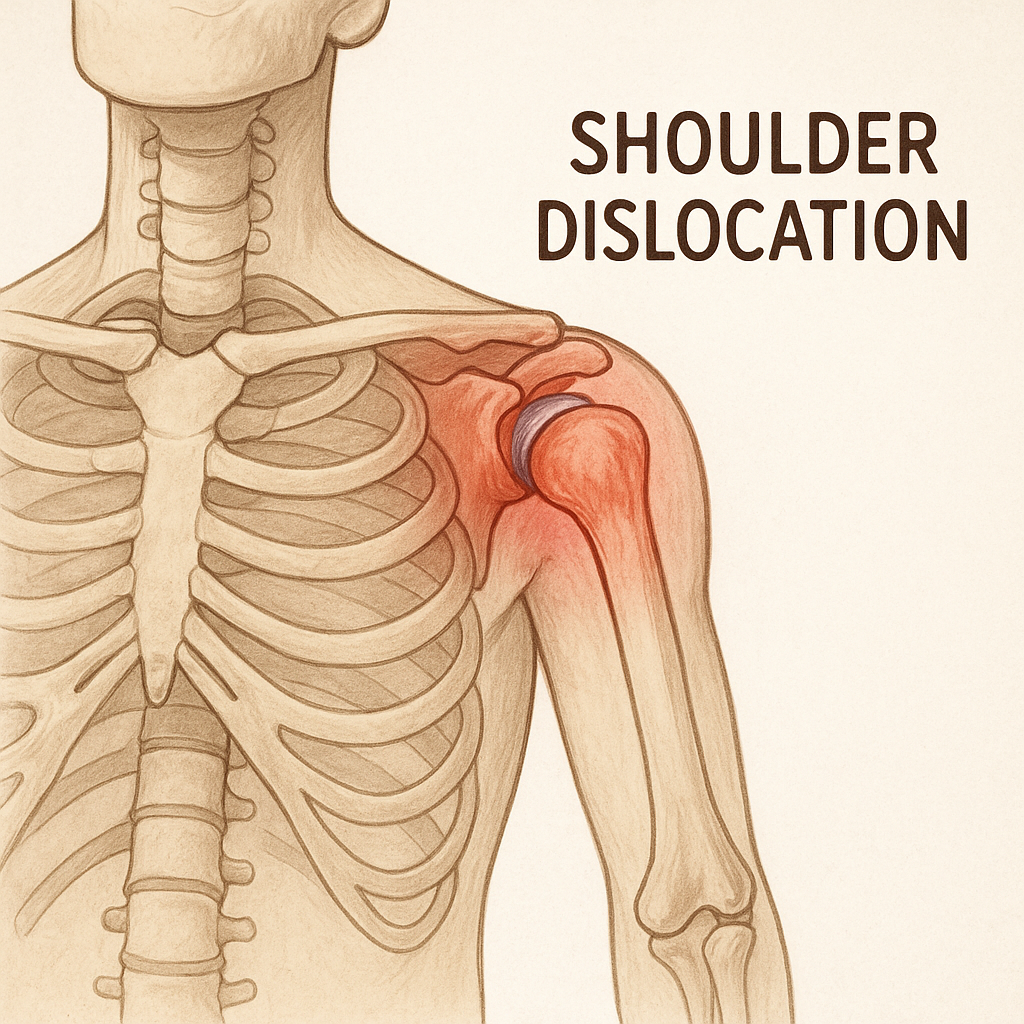
A shoulder dislocation occurs when the humeral head is forcibly displaced from the glenoid socket of the scapula. It is the most common large joint dislocation, particularly affecting athletes and physically active individuals. The majority of dislocations are anterior (forward), but posterior and inferior dislocations can also occur.
Once a shoulder has been dislocated, the surrounding soft tissues—especially the capsular ligaments and labrum—can become stretched or torn. This damage compromises the stability of the joint and predisposes patients to recurrent dislocations or a condition known as chronic shoulder instability.
Common Causes and Risk Factors for Recurrence
Recurrent shoulder instability often results from:
-
Inadequate healing of the joint capsule and glenohumeral ligaments
-
Damage to the labrum (Bankart lesion)
-
Capsular laxity or redundancy
-
Muscle imbalance or proprioceptive dysfunction
-
Premature return to activity without proper rehabilitation
Young, active individuals are particularly prone to recurrent dislocations and instability, with recurrence rates as high as 80-90% in those under 20 years old.
Traditional Management and Its Limitations
Conventional treatment approaches for shoulder dislocation and instability include:
-
Immobilization in a sling for several weeks
-
Physical therapy to restore range of motion and strengthen rotator cuff muscles
-
Surgical intervention (e.g., Bankart repair or capsular shift) for recurrent instability
While these options can be effective, they have limitations:
-
Immobilization does not restore ligament integrity
-
Rehab alone cannot tighten stretched ligaments
-
Surgery carries risks including infection, stiffness, nerve damage, or failure to resolve instability
Many patients seek non-surgical options that target the underlying soft tissue laxity to stabilize the shoulder.
What is Prolotherapy?
Prolotherapy is a regenerative injection therapy that stimulates the body’s natural healing processes to repair and strengthen damaged ligaments and tendons. The name derives from "proliferative therapy," referring to its goal of promoting tissue proliferation.
The most commonly used prolotherapy solution is a hypertonic dextrose solution (typically 15–25%) mixed with a local anesthetic such as lidocaine.
How It Works
When injected into ligamentous or capsular structures, the dextrose solution causes a controlled inflammatory response. This process:
-
Activates fibroblasts
-
Stimulates collagen synthesis
-
Leads to thickening and strengthening of ligaments
-
Restores joint stability
Unlike corticosteroid injections, which reduce inflammation but can weaken connective tissue over time, prolotherapy builds structural strength.
Treating Shoulder Instability with Prolotherapy
In patients with post-dislocation instability, prolotherapy targets the glenohumeral ligaments, joint capsule, and rotator cuff insertions to tighten the joint and prevent future dislocations.
Common injection sites include:
-
Anterior, inferior, and posterior glenohumeral ligaments
-
Middle glenohumeral ligament (MGHL)
-
Posterior capsule (for posterior instability)
-
Rotator interval region
-
Long head of biceps anchor (if involved)
By treating these areas, prolotherapy helps restore the biomechanical integrity of the joint capsule, thereby reducing:
-
Pain
-
Recurrent subluxation or dislocation
-
Weakness
-
Activity limitations
Ideal Candidates for Prolotherapy
Prolotherapy may be appropriate for patients who:
-
Have residual instability or discomfort after a shoulder dislocation
-
Show evidence of ligament laxity on physical exam
-
Have failed to achieve stability through physical therapy alone
-
Want to avoid surgery
-
Have generalized ligamentous laxity or hypermobility (e.g., Ehlers-Danlos)
It is often most effective in those with functional instability (ligament laxity) rather than mechanical instability from severe labral tears.
Treatment Protocol
Initial Evaluation
Before beginning prolotherapy, a thorough evaluation is necessary to:
-
Confirm the diagnosis of instability
-
Identify affected structures
-
Rule out complete tears requiring surgery
-
Use imaging (ultrasound or MRI) as needed
Injection Sessions
-
Injections are administered every 3 to 4 weeks
-
A typical course involves 3 to 6 treatments, depending on severity
-
Each session may involve 4 to 8 injections around the shoulder
-
Performed with local anesthetic; minimal downtime
Post-Injection Guidelines
-
Mild soreness is common for 24–48 hours
-
Avoid NSAIDs (they may inhibit the desired inflammatory response)
-
Light activity is permitted within a few days
-
Rehab exercises can continue throughout prolotherapy treatments
Evidence Supporting Prolotherapy in Shoulder Instability
While large randomized controlled trials specifically for shoulder instability are limited, several studies and clinical observations support prolotherapy's benefits:
-
Hauser et al. (2016): Comprehensive review showing prolotherapy improves pain and function across various ligament injuries, including the shoulder.
-
Reeves KD (1995): Animal studies demonstrating significant increases in ligament mass and strength after prolotherapy.
-
Klein et al. (2015): Showed improved joint stability in patients with glenohumeral instability after prolotherapy.
-
Lyftogt J (2005): Clinical observations of reduced recurrence rates and improved function with regenerative injection therapy.
Additionally, many sports medicine and physical medicine physicians report consistent real-world success in stabilizing post-dislocation shoulders.
Benefits of Prolotherapy Compared to Surgery
| Feature | Surgery | Prolotherapy |
|---|---|---|
| Invasive | Yes | No |
| Recovery Time | 4–6 months | Minimal |
| Tissue Regeneration | No (repair or resection only) | Yes (stimulates collagen) |
| Recurrent Dislocation Risk | Still possible | Reduced with proper treatment |
| Cost | High | Lower |
Prolotherapy offers a low-risk, natural option to promote healing and restore shoulder stability without the risks or recovery time of surgery.
Complementary Regenerative Therapies: PRP and Peptides
Platelet-Rich Plasma (PRP)
PRP involves injecting a concentration of the patient’s own platelets into damaged tissue to stimulate healing. Platelets contain powerful growth factors that promote:
-
Fibroblast activity
-
Collagen synthesis
-
Angiogenesis
In cases of moderate to severe instability or labral irritation, PRP can be used alongside or after prolotherapy to accelerate healing.
Peptide Therapy
Peptides are short amino acid chains that act as biological signals to regulate healing and inflammation. Specific peptides that can support shoulder ligament repair include:
-
BPC-157: Enhances healing of ligaments, tendons, and joint capsules
-
TB-500 (Thymosin Beta-4): Stimulates tissue regeneration and angiogenesis
-
GHK-Cu: Improves collagen remodeling and reduces inflammation
At Revolution Health & Wellness, we offer personalized peptide protocols to augment musculoskeletal recovery and optimize outcomes alongside prolotherapy.
Real-World Outcomes and Testimonials
Many patients report measurable improvements in pain, strength, and joint security within 1–2 months of starting prolotherapy. Typical outcomes include:
-
50–70% reduction in pain within 3 sessions
-
Fewer instances of shoulder slipping or subluxation
-
Improved ability to lift, press, or perform overhead movements
-
Reduced fear of reinjury
"I dislocated my shoulder twice in high school football and was told surgery was my only option. After prolotherapy and peptides, my shoulder feels stronger than it has in years. I'm back in the gym without fear." – Blake M., Tulsa, OK
Why Choose Revolution Health for Shoulder Prolotherapy?
Dr. Chad Edwards and the team at Revolution Health & Wellness in Tulsa, OK specialize in cutting-edge regenerative treatments for musculoskeletal injuries. Dr. Edwards has advanced training in prolotherapy, PRP, and peptide therapy to help patients avoid unnecessary surgery and recover naturally.
We offer:
-
Ultrasound-guided shoulder injections if needed
-
Evidence-based protocols
-
Individualized rehab and peptide support
Whether you’re recovering from your first dislocation or struggling with chronic instability, our mission is to restore shoulder strength from the inside out.
Take Control of Your Shoulder Health Today
If shoulder instability is interfering with your active lifestyle, you don’t have to settle for long-term pain or rush into surgery. Prolotherapy offers a regenerative, patient-centered solution to rebuild joint integrity and keep you moving strong.
Schedule your consultation at Revolution Health & Wellness to learn more about prolotherapy for post-dislocation shoulder healing and explore your personalized recovery plan.
References
-
Hauser RA, et al. A review of the clinical and basic science evidence supporting prolotherapy for ligament and tendon injuries. Open Access J Sports Med. 2016.
-
Reeves KD. Prolotherapy: Basic science, clinical studies, and technique. Phys Med Rehabil Clin N Am. 1995.
-
Klein RG, Eek BC. Prolotherapy for shoulder instability. J Back Musculoskelet Rehabil. 2015.
-
Lyftogt J. Prolotherapy for soft tissue injuries and arthritis: a clinical approach. Pain Med. 2005.
-
Mishra A, et al. Platelet-rich plasma: Current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009.
-
Szykula C, et al. The use of BPC-157 in healing soft tissue injuries: A review. J Regen Biol Med. 2021.
-
Raj NB, et al. Clinical applications of peptide therapies in orthopedic injuries. Curr Pharm Des. 2020.