The Most Important Serum Lab Markers for Optimal Bone Health and Osteoporosis Prevention
Introduction
When most people think of bone health, they think of calcium and maybe vitamin D. While these nutrients are indeed critical, bone strength is far more complex. Bones are living tissue, constantly undergoing remodeling through the coordinated actions of osteoclasts (bone breakdown) and osteoblasts (bone building).
To maintain optimal bone density and reduce the risk of osteoporosis, it’s essential to monitor the body’s internal environment. This is where serum lab markers play a powerful role. Blood tests can reveal nutrient levels, hormone status, mineral balance, and metabolic activity—all factors that directly impact bone strength and fracture risk.
In this article, we’ll cover the key serum lab markers for bone health, why they matter, and how they fit into a proactive approach to osteoporosis prevention and treatment.
Why Serum Lab Testing Matters for Bone Health
Bone density scans like DEXA provide a snapshot of current bone strength. However, they do not reveal the biological processes driving bone loss or bone building. Serum lab markers, on the other hand:
-
Detect underlying causes of low bone density.
-
Identify nutritional deficiencies that weaken bones.
-
Highlight hormonal imbalances that accelerate bone loss.
-
Guide treatment decisions and monitor response to therapy.
When combined with imaging, lifestyle assessment, and family history, serum labs provide a complete picture of bone health.
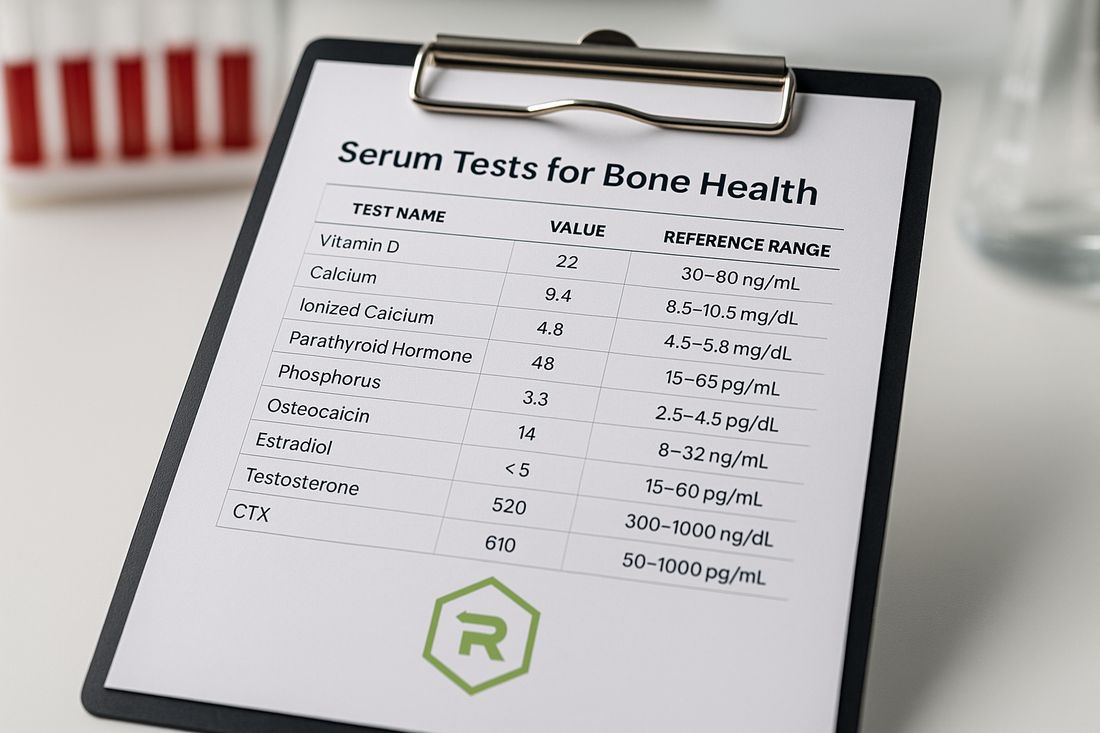
Key Serum Markers for Bone Health
1. Vitamin D (25-hydroxyvitamin D)
-
Why it matters: Vitamin D is essential for calcium absorption in the gut. Without adequate vitamin D, even high calcium intake cannot support bone mineralization.
-
Optimal range: Most experts recommend 40–60 ng/mL for bone and overall health. Levels below 30 ng/mL are associated with increased osteoporosis risk.
-
Deficiency risks: Weak bones, muscle weakness, increased falls, higher fracture risk.
2. Calcium
-
Why it matters: Calcium is the main mineral component of bone, critical for bone density. Serum calcium reflects tightly regulated blood levels but doesn’t always reveal total calcium status.
-
Optimal range: 8.6–10.2 mg/dL (varies by lab).
-
Key note: Low serum calcium often reflects vitamin D deficiency, parathyroid disorders, or kidney dysfunction rather than poor intake alone.
3. Ionized Calcium
-
Why it matters: This is the active, “free” calcium in the blood not bound to proteins. It provides a more accurate reflection of calcium status than total calcium.
-
Clinical use: Helpful in evaluating parathyroid function and bone metabolism disorders.
4. Parathyroid Hormone (PTH)
-
Why it matters: PTH regulates calcium and phosphorus balance. Elevated PTH increases bone resorption (osteoclast activity), which can weaken bone.
-
Conditions linked to abnormal PTH:
-
Primary hyperparathyroidism → bone loss, kidney stones.
-
Secondary hyperparathyroidism → often due to vitamin D deficiency or chronic kidney disease.
-
5. Phosphorus
-
Why it matters: Works with calcium to form hydroxyapatite crystals in bone. Both high and low phosphorus can negatively impact bone mineralization.
-
Optimal range: 2.5–4.5 mg/dL.
-
Concerns: High phosphorus is often seen in kidney disease; low phosphorus may impair bone strength.
6. Magnesium
-
Why it matters: Magnesium is required for vitamin D activation and calcium metabolism. Low magnesium disrupts PTH secretion and impairs bone quality.
-
Optimal range: 1.8–2.4 mg/dL, though functional medicine often targets higher-normal values for optimal health.
-
Deficiency causes: Poor diet, GI disorders, diuretic use, alcohol excess.
7. Alkaline Phosphatase (Bone-specific isoenzyme)
-
Why it matters: Alkaline phosphatase (ALP) is an enzyme produced by osteoblasts during bone formation. High levels may indicate rapid bone turnover, fracture healing, or bone disease.
-
Clinical use: Elevated bone-specific ALP can signal Paget’s disease, osteomalacia, or high turnover osteoporosis.
8. Osteocalcin
-
Why it matters: A protein secreted by osteoblasts, osteocalcin is considered a marker of bone formation.
-
Uses: Helps monitor anabolic therapies (like teriparatide) and overall osteoblast activity.
9. C-terminal Telopeptide (CTX) and N-terminal Telopeptide (NTX)
-
Why they matter: These are markers of collagen breakdown and reflect bone resorption. High levels indicate rapid bone loss.
-
Uses:
-
Detecting high-turnover osteoporosis.
-
Monitoring response to anti-resorptive therapies (like bisphosphonates or denosumab).
-
10. Estradiol (Women)
-
Why it matters: Estrogen protects bone by reducing osteoclast activity. After menopause, declining estrogen accelerates bone loss.
-
Optimal range: For bone protection, estradiol levels above 40 pg/mL are often considered protective.
-
Clinical relevance: Women with low estradiol are at significantly higher risk for osteoporosis.
11. Testosterone (Men)
-
Why it matters: Testosterone supports bone density directly and through conversion to estrogen. Men with low testosterone (hypogonadism) have increased fracture risk.
-
Optimal range: Varies by age but generally 500–800 ng/dL for healthy men.
-
Clinical use: Low levels may prompt testosterone replacement therapy to support bone health.
12. Thyroid-Stimulating Hormone (TSH) and Free T4/T3
-
Why it matters: Thyroid hormones influence bone turnover.
-
Hyperthyroidism accelerates bone resorption, leading to osteoporosis.
-
Subclinical hyperthyroidism (low TSH with normal T4/T3) is also a risk factor.
-
-
Optimal balance: Normal thyroid function supports bone stability.
13. Cortisol
-
Why it matters: Chronically elevated cortisol (as in Cushing’s syndrome or long-term steroid use) increases bone breakdown and reduces bone formation.
-
Clinical use: Serum or salivary cortisol can identify adrenal imbalances contributing to bone loss.
14. Homocysteine
-
Why it matters: High homocysteine levels are linked to reduced bone quality and higher fracture risk.
-
Mechanism: Elevated homocysteine may interfere with collagen crosslinking in bone.
-
Interventions: Folate, B6, and B12 supplementation can reduce homocysteine.
15. Insulin and Glucose (Metabolic Markers)
-
Why they matter: Insulin resistance and poorly controlled diabetes impair bone quality and increase fracture risk, even at normal bone density.
-
Labs to monitor: Fasting glucose, insulin, and HbA1c.
16. C-reactive Protein (CRP) and Inflammatory Markers
-
Why they matter: Chronic inflammation accelerates bone resorption. High CRP is linked to osteoporosis and fracture risk.
-
Clinical use: Elevated CRP suggests systemic inflammation that should be addressed for bone health.
Advanced Markers for Specialized Cases
-
Fibroblast Growth Factor-23 (FGF-23): Regulates phosphate metabolism, studied in kidney disease.
-
Sclerostin: Produced by osteocytes, inhibits bone formation.
-
Procollagen Type I N-Terminal Propeptide (P1NP): Marker of bone formation, useful in monitoring anabolic therapy.
These are less common but increasingly used in research and specialized care.
Using Serum Labs to Guide Bone Health Strategies
Once serum lab results are available, they can guide personalized interventions:
-
Low vitamin D: Supplementation with D3 + K2 for proper calcium utilization.
-
Low calcium or magnesium: Correct with dietary changes or supplements like Multi-Mineral.
-
Low estrogen or testosterone: Consider hormone replacement therapy under supervision.
-
High resorption markers (CTX, NTX): Use anti-resorptive medications or peptides to slow bone loss.
-
Inflammation or cortisol excess: Address lifestyle, stress, and targeted supplementation (e.g., Curcumin Complex).
Conclusion
Bone health is complex, but with the right tools, it can be measured, monitored, and optimized. Serum lab markers provide critical insight into nutritional status, hormone balance, and metabolic processes that influence bone remodeling.
By integrating these labs into a comprehensive evaluation—alongside imaging like DEXA and lifestyle assessment—we can detect risks early, tailor interventions, and ultimately prevent fractures and osteoporosis.
Strong bones don’t just happen with age—they are built through data-driven, proactive healthcare.
Call to Action
At Revolution Health, we go beyond standard labs to assess the full range of markers that influence bone health. If you want to know your true risk for osteoporosis and how to prevent it, schedule a Core Health Assessment with our team today. Together, we’ll create a plan that keeps your bones—and your life—strong and resilient.
References
-
Eastell R, et al. “Biochemical markers of bone turnover and their clinical use in osteoporosis.” Osteoporosis Int, 2018.
-
Holick MF. “Vitamin D deficiency.” NEJM, 2007.
-
Naylor KE, et al. “Biochemical markers of bone turnover in osteoporosis.” Clin Chim Acta, 2012.
-
Khosla S, et al. “Estrogen and bone: insights from estrogen receptor knockout mice.” J Bone Miner Res, 2012.
-
Kanis JA, et al. “European guidance for the diagnosis and management of osteoporosis.” Osteoporosis Int, 2019.