Why Testosterone Raises Hematocrit in Some Men but Not Others
Introduction
Testosterone replacement therapy (TRT) is one of the most effective treatments for men with low testosterone. It can improve muscle mass, energy, mood, libido, and bone density. Yet, for all its benefits, one of the most common concerns with TRT is an elevated hematocrit—a measure of the percentage of red blood cells in the blood.
While a mild increase in hematocrit can be beneficial for oxygen delivery and performance, too high of a hematocrit can thicken the blood, raising the risk of clotting, stroke, or cardiovascular events. What puzzles clinicians and patients alike is that not every man experiences this side effect. Some men on testosterone develop significantly elevated hematocrit, while others remain stable even on higher doses.
So, what explains this variability? In this article, we’ll explore the science behind testosterone-induced erythrocytosis (elevated red blood cells), the individual factors that make some men more susceptible, and strategies to monitor and manage hematocrit safely during TRT.
Understanding Hematocrit and Testosterone
What Is Hematocrit?
Hematocrit (Hct) is the percentage of blood volume made up of red blood cells. Normal ranges:
-
Men: 40–52%
-
Women: 36–48%
When hematocrit rises above 52–54% in men, blood viscosity increases significantly, which may strain the cardiovascular system.
How Testosterone Affects Hematocrit
Testosterone stimulates red blood cell production through multiple mechanisms:
-
Erythropoietin (EPO) Stimulation
Testosterone boosts EPO production in the kidneys. EPO is the hormone that tells bone marrow to make more red blood cells. -
Suppression of Hepcidin
Hepcidin is a hormone that limits iron absorption. Testosterone lowers hepcidin, allowing more iron to be absorbed and used for red blood cell synthesis. -
Bone Marrow Stimulation
Testosterone directly activates bone marrow, promoting erythropoiesis (red blood cell formation).
This triple effect—more EPO, more iron availability, and more marrow activity—explains why testosterone is such a powerful driver of hematocrit.
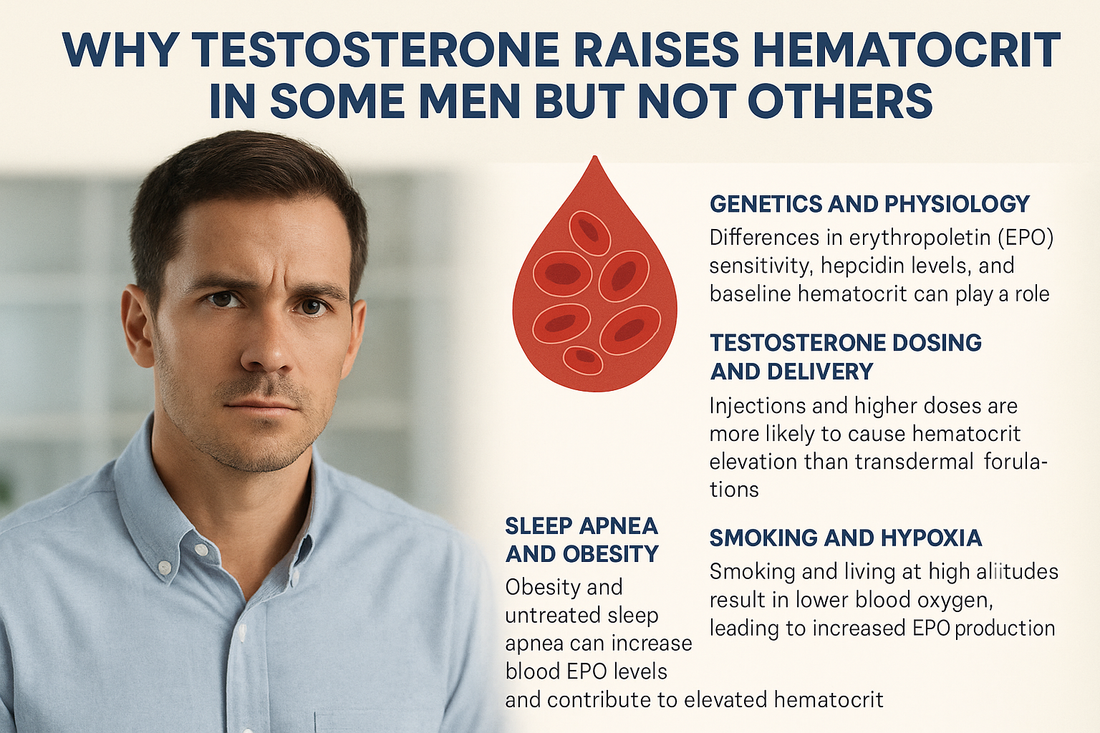
Why Do Some Men Experience High Hematocrit While Others Do Not?
1. Genetics and Baseline Physiology
-
EPO Sensitivity: Some men’s bone marrow responds more strongly to EPO than others.
-
Hepcidin Variability: Genetic differences in iron regulation can amplify or mute testosterone’s effects.
-
Baseline Hematocrit: Men who naturally run “high-normal” at baseline (e.g., Hct 48–50%) are more likely to exceed safe thresholds when starting TRT than men whose baseline is lower.
2. Age and Androgen Receptor Sensitivity
Older men may have increased sensitivity of hematopoietic (blood-forming) tissue to testosterone. Variations in androgen receptor gene polymorphisms (CAG repeat length) also change how strongly tissues respond to testosterone, including bone marrow.
3. Testosterone Formulation and Delivery Method
Not all TRT methods affect hematocrit equally:
-
Injections (especially intramuscular, long-acting): Most likely to cause hematocrit spikes because they create high serum peaks.
-
Pellets: Can cause moderate elevations depending on dose.
-
Transdermal gels/creams: Less likely to cause large hematocrit increases due to steadier hormone levels.
-
Oral formulations: Rarely used but tend to have less impact on hematocrit.
Thus, the pharmacokinetics of testosterone delivery explain some of the individual variability.
4. Body Composition and Sleep Apnea
-
Obesity and sleep apnea both increase risk of high hematocrit.
-
Obstructive sleep apnea causes intermittent hypoxia (low oxygen), which stimulates EPO and red blood cell production. TRT can worsen sleep apnea, amplifying the problem.
-
Men with higher visceral fat often have more systemic inflammation, which alters iron and hepcidin metabolism, further contributing to variability.
5. Smoking and Hypoxia
-
Smokers naturally have higher hematocrit due to carbon monoxide exposure, which reduces oxygen carrying capacity.
-
Adding TRT can push these men over the threshold.
-
Living at high altitudes has the same effect—chronic low oxygen drives red blood cell production.
6. Iron Stores and Nutrition
Men with higher iron stores (ferritin levels) have more substrate for red blood cell production when testosterone suppresses hepcidin. Conversely, men with borderline low iron may not see as dramatic an increase.
7. Dose and Duration of TRT
The relationship is dose-dependent: higher doses produce stronger stimulation of erythropoiesis. Longer duration of therapy allows hematocrit to gradually climb, typically peaking around 6–12 months.
The Clinical Risks of Elevated Hematocrit
When hematocrit rises above ~52–54%, risks increase:
-
Blood viscosity increases, making circulation sluggish.
-
Platelet activation and clotting risk rise.
-
Stroke, heart attack, and venous thromboembolism risk may increase.
-
Blood pressure can rise due to increased vascular resistance.
While the absolute risk is debated—since not all studies show high event rates—clinicians universally agree that monitoring hematocrit is essential.
Monitoring Hematocrit on Testosterone Therapy
Best practices include:
-
Baseline CBC before starting TRT.
-
Recheck at 3 months, 6 months, and annually.
-
More frequent monitoring for men on high-dose injections, those with sleep apnea, smokers, or men with prior high hematocrit.
Management Strategies When Hematocrit Rises
1. Adjust Testosterone Dose or Delivery
-
Lower the dose to reduce peaks.
-
Switch from injections to transdermal methods for steadier levels.
2. Treat Contributing Conditions
-
Evaluate and treat sleep apnea.
-
Encourage weight loss to improve oxygenation.
-
Smoking cessation is critical.
3. Address Iron and Diet
-
Avoid unnecessary iron supplementation.
-
Monitor ferritin and iron studies.
4. Therapeutic Phlebotomy
-
If hematocrit exceeds 54%, many physicians recommend phlebotomy (blood donation).
-
This reduces hematocrit quickly but must be combined with dose adjustments to prevent recurrence.
5. Optimize Cardiovascular Protection
-
Supplements like Omega 1300 can reduce inflammation and improve vascular health.
-
Curcumin Complex supports healthy blood viscosity and reduces clotting risk.
Why Monitoring Matters: Different Responses, Different Risks
The key point is that TRT is not one-size-fits-all. Two men on the exact same dose may respond very differently:
-
Man A: Baseline Hct 46%, on 100 mg testosterone weekly, hematocrit stabilizes at 49%.
-
Man B: Baseline Hct 49%, on 100 mg weekly, hematocrit rises to 55% after 6 months.
This variability reflects differences in genetics, comorbidities, oxygen status, and metabolism. That’s why personalized medicine—ongoing monitoring and adjusting therapy to the individual—is essential.
The Role of Estrogen in Hematocrit Regulation
Another layer of complexity: testosterone is aromatized to estradiol. While estrogen plays a protective role in cardiovascular health, it also influences bone marrow activity and iron metabolism. Some studies suggest that men who convert more testosterone to estrogen may experience different hematocrit responses than those who do not.
Looking Ahead: Research and Future Therapies
Researchers are actively exploring:
-
Selective androgen receptor modulators (SARMs) – which may stimulate muscle without dramatically raising hematocrit.
-
Modified testosterone formulations – to reduce hematocrit spikes.
-
Better risk stratification – using genetic markers or baseline labs to predict which men will develop erythrocytosis.
This will allow safer, more individualized TRT in the future.
Conclusion
Testosterone therapy is life-changing for men with low T—but it requires careful management. The increase in hematocrit seen in some men, but not others, reflects a complex interplay of:
-
Genetics
-
Delivery method
-
Sleep and oxygen status
-
Body composition
-
Baseline hematocrit and iron stores
For some, TRT has little effect on hematocrit. For others, levels rise rapidly and require close monitoring.
With regular blood work, smart dose adjustments, lifestyle changes, and preventive strategies, testosterone therapy can be used safely while minimizing risks.
Call to Action
If you’re on testosterone therapy—or considering starting—it’s essential to work with a clinic experienced in personalized hormone management. At Revolution Health, we specialize in hormone optimization with comprehensive monitoring, ensuring you get the benefits of testosterone while avoiding complications like high hematocrit.
Schedule your consultation today and take control of your health with a precision approach to TRT.
References
-
Bachman E, et al. “Testosterone Induces Erythrocytosis via Increased Erythropoietin and Suppressed Hepcidin.” J Clin Invest, 2014.
-
Calof OM, et al. “Adverse Events Associated With Testosterone Replacement in Middle-Aged and Older Men.” J Gerontol A Biol Sci Med Sci, 2005.
-
Braekkan SK, et al. “Hematocrit and Risk of Venous Thromboembolism.” Haematologica, 2010.
-
Morgentaler A, Traish AM. “Shifting the Paradigm of Testosterone and Prostate Cancer: The Saturation Model.” Eur Urol, 2009.
-
Snyder PJ, et al. “Effects of Testosterone Treatment in Older Men.” NEJM, 2016.
-
Ohlander SJ, et al. “Erythrocytosis Following Testosterone Therapy.” Sex Med Rev, 2018.