ApoA-I: The HDL Protein That Protects Your Heart
Introduction
Cardiovascular disease (CVD) remains the leading cause of death worldwide. For decades, physicians focused on cholesterol—particularly LDL (“bad cholesterol”) and HDL (“good cholesterol”)—as the main predictors of heart attack and stroke. But research has shown that cholesterol numbers alone don’t tell the full story.
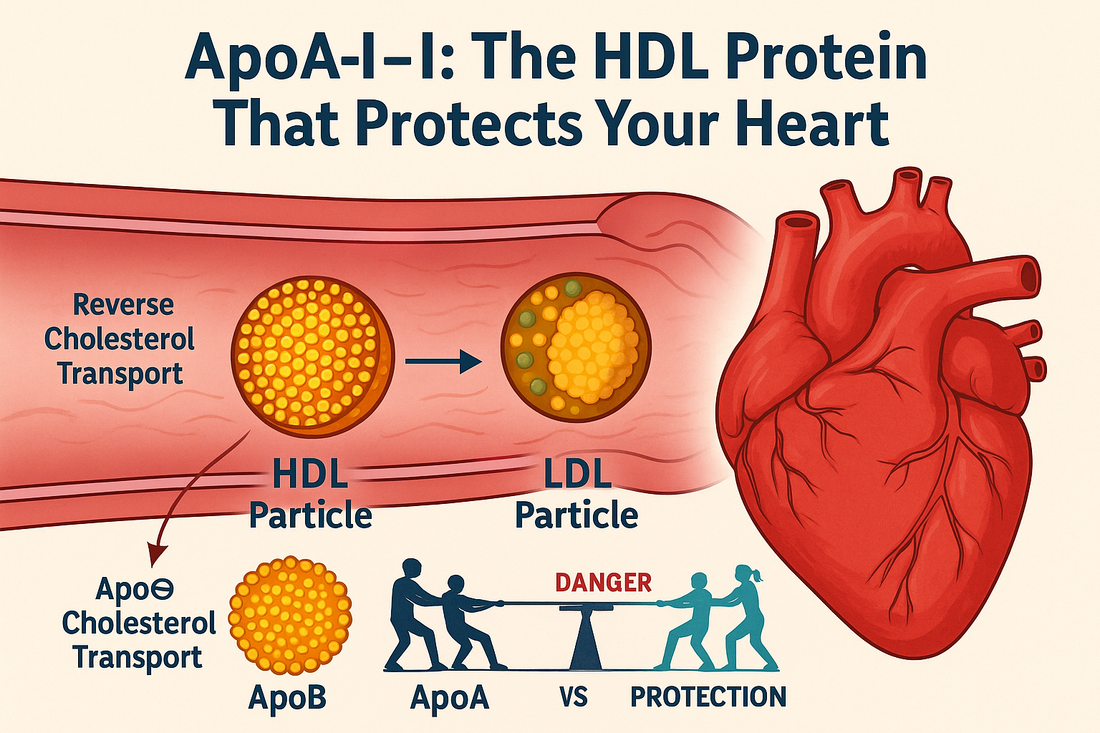
One of the most important markers in cardiovascular risk assessment is Apolipoprotein A-I (ApoA-I), the major protein of HDL particles. ApoA-I is not just a structural component; it is the driving force behind many of HDL’s protective functions, including reverse cholesterol transport, antioxidant activity, anti-inflammatory signaling, and endothelial support.
In this article, we’ll cover:
-
What ApoA-I is and why it matters
-
How it relates to HDL cholesterol
-
How it is measured and interpreted in labs
-
The ApoB:ApoA-I ratio as a powerful cardiovascular risk marker
-
Factors that lower ApoA-I levels
-
Evidence-based strategies to improve ApoA-I with lifestyle, supplements, and therapies
By the end, you’ll understand why ApoA-I is a cornerstone biomarker in advanced cardiovascular testing—something we routinely use at Revolution Health.
What is ApoA-I?
Apolipoprotein A-I (ApoA-I) is the main protein component of HDL cholesterol particles, making up about 70% of HDL’s total protein content. Produced in the liver and intestine, ApoA-I plays a central role in lipid metabolism.
Functions of ApoA-I include:
-
Reverse cholesterol transport: helping remove cholesterol from artery walls and delivering it back to the liver for excretion.
-
Activating LCAT (lecithin cholesterol acyltransferase): an enzyme that esterifies cholesterol, allowing HDL particles to mature and expand.
-
Anti-inflammatory effects: reducing cytokine activity and oxidative stress within blood vessels.
-
Antioxidant properties: preventing LDL from becoming oxidized (oxLDL), a key driver of atherosclerosis.
-
Endothelial protection: improving nitric oxide availability and vascular flexibility.
In short, ApoA-I is what gives HDL its “good cholesterol” benefits.
ApoA-I vs. HDL Cholesterol: What’s the Difference?
Traditional testing measures HDL cholesterol (HDL-C), the cholesterol content carried inside HDL particles. While HDL-C has long been considered protective, studies show it’s not always reliable:
-
Some people have high HDL-C but still develop heart disease, because their HDL is dysfunctional.
-
Others may have low HDL-C but high ApoA-I levels, meaning their HDL particles are effective at doing their job.
Why ApoA-I is Better
-
HDL-C = cargo (cholesterol inside HDL particles).
-
ApoA-I = engine (the protein that makes HDL function).
That’s why measuring ApoA-I directly provides a clearer picture of HDL’s protective power.
How ApoA-I is Measured
ApoA-I is measured through a blood test, usually as part of an advanced cardiovascular panel.
-
Normal reference ranges:
-
Men: 110–180 mg/dL
-
Women: 120–200 mg/dL
-
-
Low ApoA-I: <115 mg/dL in men, <125 mg/dL in women (depending on lab standards).
Since ApoA-I is inversely related to cardiovascular risk, higher levels are generally protective.
The ApoB:ApoA-I Ratio
One of the most powerful ways to use ApoA-I is in combination with Apolipoprotein B (ApoB), the protein that represents atherogenic particles such as LDL and VLDL.
-
ApoB = “bad particles” (number of cholesterol-delivery vehicles that can enter artery walls).
-
ApoA-I = “good particles” (removal and cleanup crew).
The ApoB:ApoA-I ratio reflects the balance between cholesterol deposition and removal.
-
High ratio = more risk (more ApoB relative to ApoA-I).
-
Low ratio = lower risk (more ApoA-I to counterbalance ApoB).
Studies show the ApoB:ApoA-I ratio is one of the best predictors of heart attack risk, outperforming LDL-C, HDL-C, and even non-HDL cholesterol.
What Causes Low ApoA-I Levels?
Several conditions and lifestyle factors can lower ApoA-I:
-
Genetic Factors
-
ApoA-I deficiency (rare)
-
ApoA-I mutations such as ApoA-I Milano (unique variant with protective function despite low levels)
-
-
Metabolic Syndrome & Diabetes
-
Insulin resistance lowers HDL function and ApoA-I expression.
-
-
Obesity & Poor Diet
-
High refined carbs, trans fats, and processed foods reduce ApoA-I.
-
-
Chronic Inflammation
-
Systemic inflammation suppresses ApoA-I synthesis.
-
-
Smoking
-
Smoking decreases ApoA-I levels and impairs HDL’s antioxidant function.
-
-
Sedentary Lifestyle
-
Physical inactivity leads to lower ApoA-I and dysfunctional HDL.
-
Clinical Importance of ApoA-I
-
Low ApoA-I levels are associated with:
-
Increased risk of coronary artery disease
-
Stroke
-
Metabolic syndrome
-
Type 2 diabetes
-
Accelerated atherosclerosis
-
-
High ApoA-I levels are generally protective, though excessively high levels (rare) may occur in certain genetic conditions.
How to Improve ApoA-I Levels
The good news: ApoA-I levels and HDL function can be improved with targeted interventions.
1. Lifestyle Changes
-
Exercise: Aerobic exercise increases ApoA-I and HDL function. Resistance training adds further benefit.
-
Nutrition:
-
Mediterranean diet (olive oil, nuts, fish, vegetables) improves ApoA-I expression.
-
Reduce processed foods and sugars.
-
Include omega-3–rich foods (salmon, sardines, flaxseed).
-
-
Weight management: Losing excess visceral fat raises ApoA-I and improves the ApoB:ApoA-I ratio.
-
Quit smoking: Increases ApoA-I and restores HDL function.
2. Supplements
-
Omega 1300: Increases ApoA-I, improves HDL particle quality, and reduces vascular inflammation.
-
Curcumin Complex: Anti-inflammatory support, helps HDL function.
-
CoQ10 Omega: Supports mitochondrial health and reduces oxidative stress.
-
ActiveMulti: Ensures micronutrient sufficiency for cardiovascular repair.
-
Niacin (Vitamin B3): Can raise ApoA-I, though use is limited by side effects.
3. Peptide Therapy
While research is ongoing, certain peptides may support ApoA-I and HDL function indirectly:
-
MOTS-c: Improves mitochondrial function and insulin sensitivity, lowering metabolic stress on lipids.
-
Tesamorelin: Reduces visceral fat, indirectly improving ApoA-I and HDL function.
-
CJC-1295 + Ipamorelin: Support growth hormone release, improving lipid metabolism and vascular repair.
4. Medications
-
Statins: modestly raise ApoA-I, though their main benefit is lowering ApoB particles.
-
Fibrates: increase ApoA-I production and raise HDL-C.
-
CETP inhibitors (investigational): can raise ApoA-I significantly, though not yet standard therapy.
Key Takeaways
-
ApoA-I is the primary protein of HDL and the true driver of “good cholesterol.”
-
It is critical for reverse cholesterol transport, vascular protection, and anti-inflammatory activity.
-
Measuring ApoA-I provides a more reliable predictor of heart health than HDL cholesterol alone.
-
The ApoB:ApoA-I ratio is one of the strongest indicators of cardiovascular risk.
-
Low ApoA-I can result from genetics, inflammation, obesity, diabetes, smoking, and poor lifestyle habits.
-
Improving ApoA-I involves lifestyle changes, supplements like Omega 1300 and Curcumin Complex, peptide therapies, and in some cases, medications.
At Revolution Health, we integrate ApoA-I testing into our advanced cardiovascular assessment protocols—helping patients go beyond standard cholesterol panels to truly understand their risk and take steps to prevent heart disease before it starts.
References
-
Franceschini G. Apolipoprotein A-I: a multifunctional protein at the interface of lipid metabolism and atherosclerosis. Atherosclerosis. 2001.
-
Kontush A, Chapman MJ. Antiatherogenic function of HDL particle subpopulations: focus on antioxidative activities. Curr Opin Lipidol. 2010.
-
Walldius G, Jungner I. The ApoB/ApoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy. J Intern Med. 2006.
-
Tall AR. Cholesterol efflux pathways and other potential mechanisms involved in the athero-protective effect of high density lipoproteins. J Intern Med. 2008.
-
Barter PJ, Rye KA. The rationale for using apoA-I as a clinical marker of cardiovascular risk. Clin Lipidol. 2012.
-
Gordon DJ, Rifkind BM. High-density lipoprotein—the clinical implications of recent studies. N Engl J Med. 1989.
-
Nordestgaard BG, Langsted A, Mora S, et al. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications. Eur Heart J. 2016.
-
Schaefer EJ, Santos RD, Asztalos BF. Markers of HDL functionality. Curr Opin Lipidol. 2010.
-
Rosenson RS, Brewer HB Jr, Davidson WS, et al. Cholesterol efflux and atheroprotection: advancing the concept of HDL functionality. Circulation. 2012.