Deoxypyridinoline and Bone Health: What This Marker Reveals About Your Skeleton
Introduction
Bone health is about much more than avoiding fractures. Your skeleton is a living, dynamic organ system that undergoes constant remodeling—old bone is broken down, and new bone is built. When this delicate balance tips toward excessive breakdown, conditions such as osteopenia and osteoporosis can develop, leading to increased fracture risk and declining quality of life.
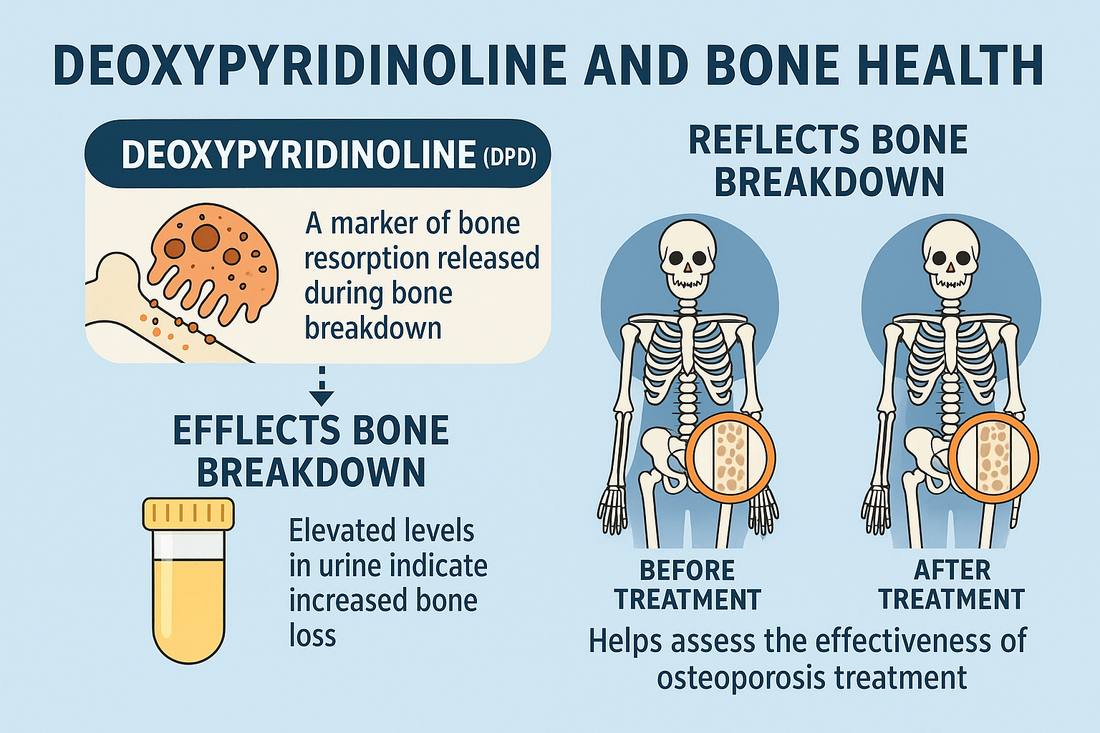
One of the most useful ways to assess this balance is by measuring deoxypyridinoline (DPD), a collagen crosslink that appears in the urine when bone is being resorbed. In other words, DPD is a biochemical marker of bone breakdown. By understanding how it works, clinicians and patients can gain valuable insight into bone health, monitor disease progression, and evaluate treatment effectiveness.
In this article, we’ll explore:
-
What deoxypyridinoline is and how it relates to bone turnover
-
How DPD testing works and why it’s clinically important
-
The role of DPD in osteoporosis, menopause, and other conditions
-
Strategies to lower excessive bone resorption and strengthen bone
What Is Deoxypyridinoline?
A Collagen Crosslink
Deoxypyridinoline is a crosslink compound formed in the collagen fibers of bone. Collagen gives bone its flexibility and framework, while minerals like calcium and phosphate provide hardness.
When bone tissue is broken down by osteoclasts (the cells responsible for resorption), collagen fibers are degraded and deoxypyridinoline is released into circulation. Because the body does not reuse or metabolize DPD, it is excreted in the urine—making it a direct indicator of bone resorption.
Why It Matters
High levels of urinary DPD indicate accelerated bone breakdown, which can occur in:
-
Osteoporosis and osteopenia
-
Postmenopausal bone loss
-
Hyperparathyroidism
-
Certain cancers with bone metastases
-
Chronic corticosteroid use
Monitoring DPD levels provides early warning of skeletal imbalance, often before bone density scans reveal significant changes.
Bone Remodeling: The Balance of Formation and Resorption
To understand DPD’s role, it helps to review how bones remodel:
-
Osteoclasts resorb bone by dissolving minerals and breaking down collagen.
-
Osteoblasts rebuild bone by laying down new collagen matrix and mineralizing it.
-
A healthy adult renews 5–10% of bone mass annually through this cycle.
When resorption outpaces formation, bone density declines. Elevated urinary DPD means osteoclast activity is too high—an early red flag for osteoporosis and fracture risk.
How Is Deoxypyridinoline Measured?
Urinary DPD Testing
DPD is measured in urine, usually as:
-
24-hour collection (gold standard, but less convenient)
-
First morning void sample (more practical for patients)
Results are expressed as DPD/creatinine ratio to account for urine concentration.
Interpretation
-
Normal levels: Reflect balanced bone turnover
-
Elevated levels: Suggest increased bone resorption
-
Low levels: May indicate effective anti-resorptive therapy or low osteoclast activity
Because bone turnover varies with age, sex, and menopausal status, results must be compared against reference ranges.
DPD and Osteoporosis
Early Detection
Osteoporosis is often called the “silent disease” because bone loss occurs without symptoms until a fracture happens. DEXA scans measure bone mineral density (BMD), but they don’t show active turnover.
That’s where DPD adds value—it reflects real-time bone resorption activity, enabling earlier detection of excessive loss.
Monitoring Treatment
DPD is especially useful for tracking response to osteoporosis therapies:
-
Bisphosphonates (alendronate, risedronate): Suppress osteoclast activity, lowering DPD within 3–6 months.
-
Denosumab: A potent anti-resorptive agent that reduces DPD significantly.
-
Hormone replacement therapy (HRT): Decreases DPD in postmenopausal women by stabilizing bone turnover.
-
Anabolic agents (teriparatide, abaloparatide, romosozumab): Increase bone formation, but DPD can remain elevated initially before stabilizing.
By following DPD trends, clinicians can confirm whether a therapy is effectively slowing bone breakdown.
DPD in Postmenopausal Women
Estrogen is a key regulator of bone health. After menopause, estrogen levels drop sharply, leading to:
-
Increased osteoclast activity
-
Accelerated bone resorption
-
Rising urinary DPD levels
This makes DPD testing particularly valuable for postmenopausal women, helping identify those at highest risk for rapid bone loss.
Other Conditions Linked to Elevated DPD
-
Hyperparathyroidism: Excess parathyroid hormone stimulates bone resorption.
-
Cushing’s syndrome or steroid therapy: Long-term glucocorticoids accelerate bone breakdown.
-
Paget’s disease: Characterized by excessive, disorganized bone turnover.
-
Bone metastases from cancers: Tumor cells often stimulate osteoclasts, elevating DPD.
In each of these conditions, DPD acts as a biomarker of disease activity.
Lifestyle and Nutritional Influences on Bone Resorption
Excess bone breakdown is not only disease-driven. Lifestyle plays a huge role in determining DPD levels and long-term skeletal health.
Risk Factors That Increase Bone Resorption
-
Low calcium and vitamin D intake
-
Sedentary lifestyle
-
Smoking and alcohol use
-
Chronic stress and cortisol elevation
-
High soft drink or caffeine consumption
Protective Lifestyle Measures
-
Weight-bearing exercise stimulates bone formation and reduces resorption.
-
Adequate dietary protein supports collagen matrix.
-
Balanced minerals—magnesium, zinc, and boron are all crucial for bone integrity.
-
Sunlight exposure or supplementation for vitamin D sufficiency.
Supplement Support for Bone Health
Several nutritional supplements support healthy bone turnover and may lower excessive resorption reflected by DPD:
-
Vitamin D3 + K2
-
Vitamin D improves calcium absorption.
-
Vitamin K2 directs calcium into bone, not arteries.
-
-
Calcium (MCHC or citrate forms)
-
Essential for bone mineralization.
-
Best taken with vitamin D and magnesium.
-
-
Magnesium
-
Supports bone structure and reduces PTH overactivity.
-
-
Collagen and amino acids
-
Provide raw materials for bone matrix.
-
-
Resveratrol and polyphenols
-
Reduce oxidative stress and osteoclast activation.
-
-
Peptides for bone health
-
BPC-157 and TB-500 may support repair and reduce inflammation.
-
CJC-1295 and Ipamorelin indirectly promote bone growth via growth hormone stimulation.
-
Integrative Approaches to Healthy Bone Remodeling
A truly comprehensive bone health strategy includes:
-
Baseline and follow-up DPD testing to track bone resorption.
-
DEXA scans to monitor bone density.
-
Personalized supplementation with vitamin D, K2, calcium, magnesium, and targeted compounds.
-
Peptide therapy when appropriate to stimulate repair and regeneration.
-
Lifestyle interventions including exercise, diet, sleep, and stress management.
By integrating biochemical markers like DPD with imaging and clinical history, practitioners can design personalized, evidence-based plans for maintaining skeletal strength.
Deoxypyridinoline vs. Other Bone Markers
There are several markers of bone turnover, but each has strengths and weaknesses:
-
NTX (N-telopeptide): Also measures collagen breakdown; less specific than DPD.
-
CTX (C-terminal telopeptide): A widely used serum marker of resorption.
-
P1NP (Procollagen type I N-terminal propeptide): Marker of bone formation.
DPD is highly specific to bone collagen (not influenced by diet or other tissues), making it one of the most reliable markers of true bone resorption.
Clinical Case Example
-
A 54-year-old postmenopausal woman presents with early osteopenia on DEXA.
-
Baseline urinary DPD is significantly elevated, indicating active resorption.
-
She begins HRT, vitamin D/K2 supplementation, and weight-bearing exercise.
-
Repeat DPD testing at 6 months shows a 40% reduction, confirming treatment effectiveness before DEXA shows major density changes.
This illustrates how DPD allows clinicians to monitor therapy success much earlier than imaging alone.
Conclusion
Deoxypyridinoline is more than just a laboratory marker—it’s a window into the dynamic process of bone remodeling. Elevated levels warn of excessive resorption long before fractures occur or density loss becomes severe.
By combining DPD testing with lifestyle strategies, targeted supplements, and appropriate medical therapies, patients can proactively protect their bones, reduce osteoporosis risk, and maintain lifelong skeletal strength.
Call to Action
At Revolution Health, we use advanced testing—including urinary deoxypyridinoline—to assess bone turnover and identify risks early. Our personalized programs combine nutrition, peptides, hormone optimization, and integrative care to strengthen your bones and protect your long-term health.
Schedule a consultation today to take control of your bone health and prevent future fractures.
References
-
Garnero P, et al. “Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment.” Osteoporosis Int, 2000.
-
Seibel MJ. “Biochemical markers of bone turnover part I: biochemistry and variability.” Clin Biochem Rev, 2005.
-
Eastell R, et al. “Biochemical markers of bone turnover and fracture risk.” Bone, 2018.
-
Wheater G, et al. “Markers of bone turnover in osteoporosis.” Clin Chim Acta, 2010.
-
Vasikaran S, et al. “Markers of bone turnover for the prediction of fracture risk and monitoring of treatment: a need for international reference standards.” Osteoporosis Int, 2011.